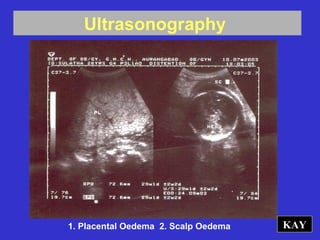
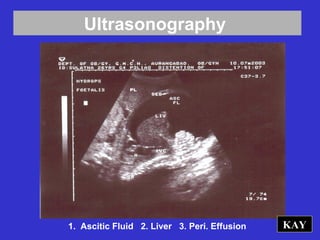
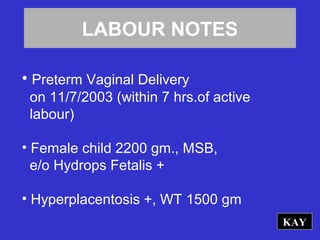
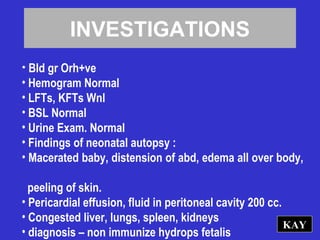
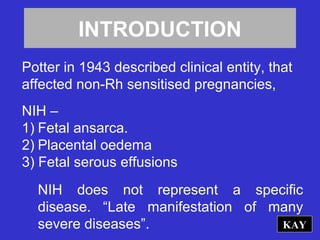
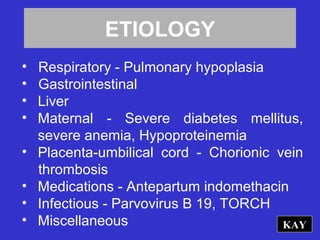
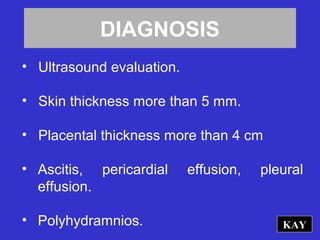
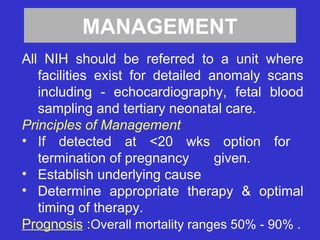
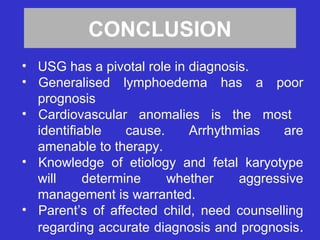
This document discusses non-immune hydrops fetalis (NIH), which causes fetal swelling. NIH has many potential causes including cardiovascular anomalies, chromosomal abnormalities, and infections. Ultrasound is used to diagnose NIH by identifying signs such as skin thickness over 5mm, placental thickness over 4cm, and fluid accumulations. The prognosis is poor, with mortality rates of 50-90%. While the underlying cause should be determined, the outcome depends on the specific condition and potential for treatment.