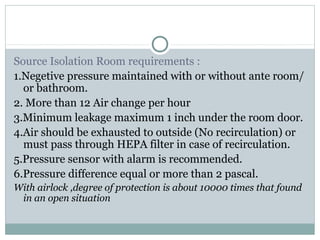
This document discusses the history and importance of isolation facilities for preventing the spread of contagious diseases. It outlines how isolation was used as early as the 18th century for diseases like smallpox. The development of germ theory in the 19th century established isolation as a key prevention strategy when treatments were not available. The document then describes the requirements and best practices for designing isolation rooms today, including engineering controls like negative or positive pressure. It emphasizes isolation can cause psychological stress for patients, so facilities should aim to minimize this.