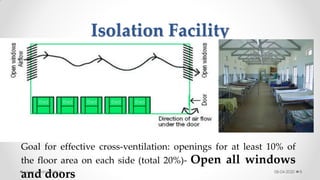
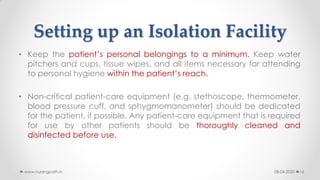
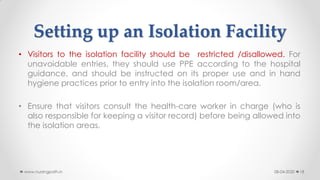
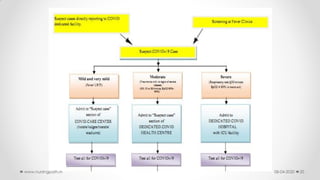
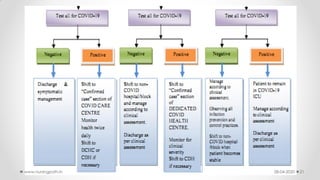
This document provides guidance for establishing an isolation facility at a district hospital to contain outbreaks, particularly for COVID-19. It outlines protocols for isolation, case management, and infection prevention, emphasizing the need for separate spaces for confirmed and suspected cases, proper PPE usage, and adherence to hygiene practices. The document also covers logistics for patient care equipment, waste disposal, and the necessity of training healthcare personnel in infection control practices.