The document provides information about strokes, including:
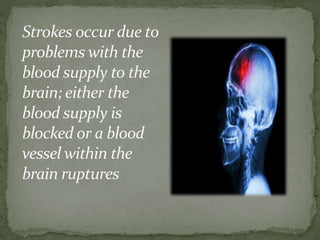
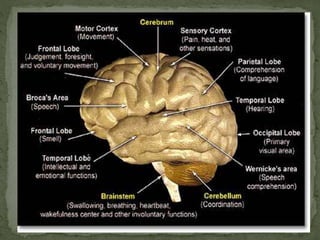
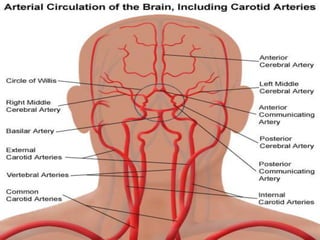
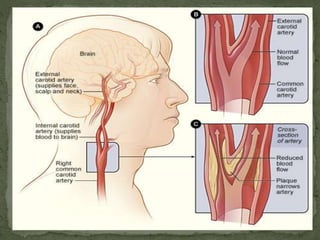
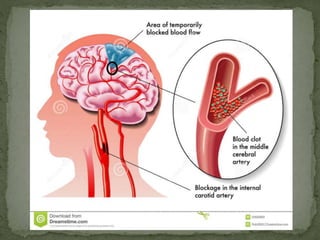
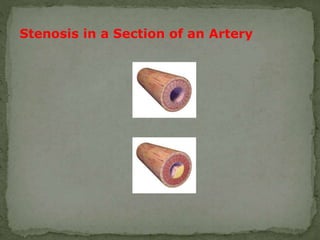
1) Strokes occur when the blood supply to the brain is interrupted or reduced, causing brain cells to die from lack of oxygen and nutrients. There are three main types of stroke: ischemic, hemorrhagic, and TIA.
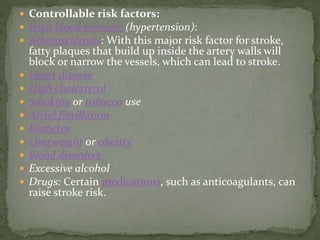
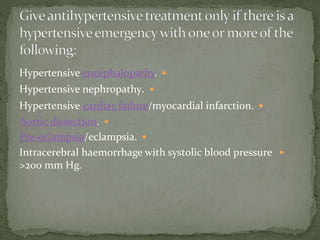
2) Risk factors for stroke include hypertension, heart disease, high cholesterol, smoking, atrial fibrillation, diabetes, overweight/obesity, blood disorders, excessive alcohol, and certain medications. Symptoms appear suddenly and include confusion, weakness, vision problems, and trouble walking or talking.
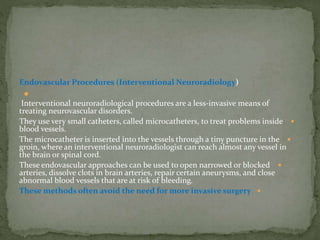
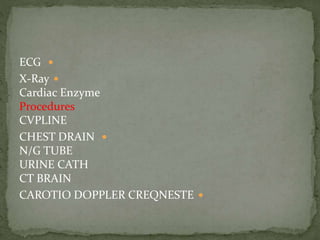
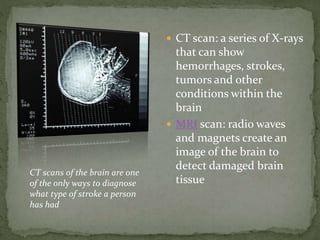
3) Diagnosis involves physical exams, blood tests, CT/MRI scans, and other specialized tests. Treatment

![Fibrinolytic therapy
Antiplatelet agents [4, 5]
Mechanical thrombectomy](https://image.slidesharecdn.com/stroke1-150424035750-conversion-gate02/85/ischemic-stroke-53-320.jpg)
![People with acute stroke should have their swallowing screened before
being given any oral food, fluid or medication.[7] Also screen
for malnutrition.
Aspirin (300 mg) should be given as soon as possible after the onset of
stroke symptoms once a diagnosis of primary haemorrhage has been
excluded.[8]Antiplatelet therapy should then be continued indefinitely.
Therapy should be delayed for 24 hours following thrombolysis.
Clopidogrel 75mg daily is recommended.[7]
Thrombolytic treatment: see separate article Thrombolytic Treatment
of Acute Ischaemic Stroke. Unless there are contra-indications,
thrombolytic treatment appears to be effective in improving prognosis
after an acute stroke.[9] Treatment withalteplase should only be given
provided that:
It is administered within four and a half hours of onset of stroke
Anticoagulants should not be started until brain imaging has excluded
haemorrhage. In patients with acute ischaemic strokesymptoms
(unless as part of a clinical trial).](https://image.slidesharecdn.com/stroke1-150424035750-conversion-gate02/85/ischemic-stroke-58-320.jpg)