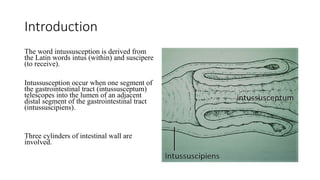
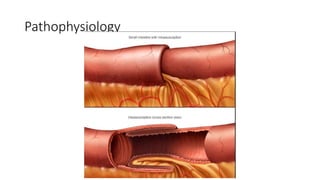
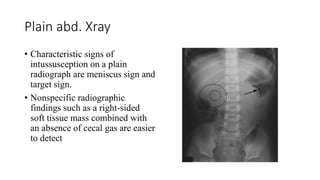
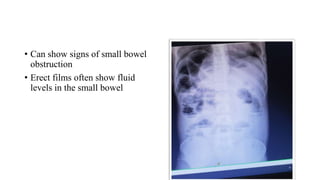
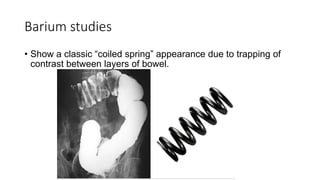
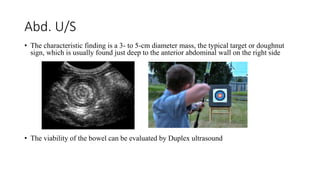
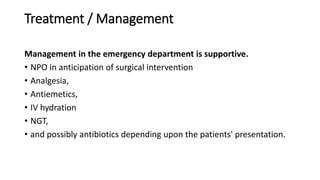
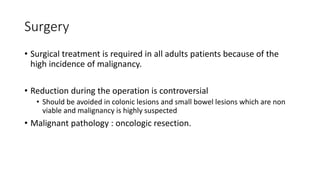
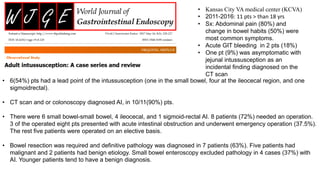
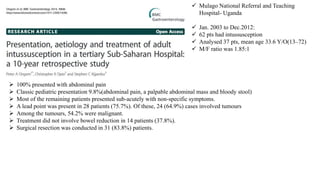
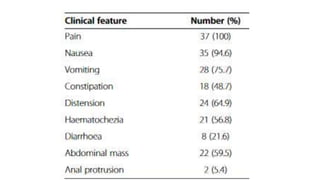
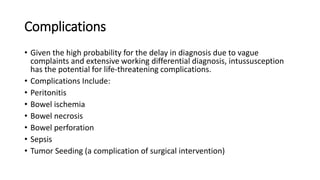
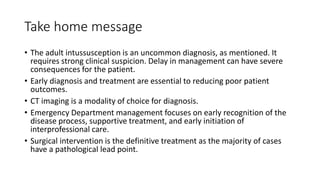
Adult intussusception is rare, accounting for 1% of small bowel obstructions. It is usually caused by an underlying pathological lead point like a tumor. CT imaging is the most sensitive test for diagnosis and can identify potential lead points. Presenting symptoms are nonspecific like abdominal pain but complications from delay in diagnosis or treatment include bowel ischemia, perforation and sepsis. Surgical intervention is usually required for definitive treatment and pathology diagnosis given the high incidence of malignancy as the lead point.