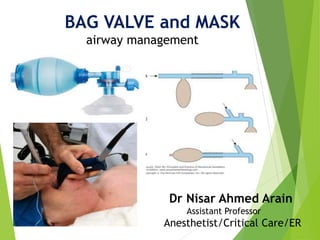
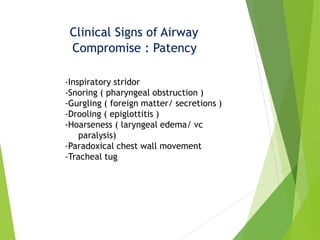
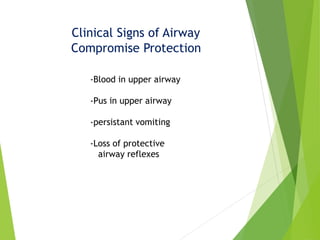
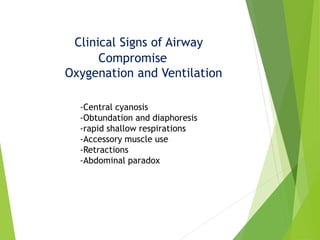
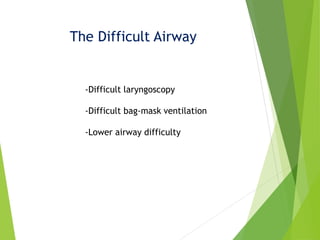
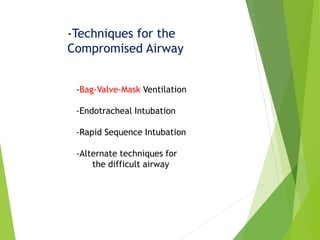
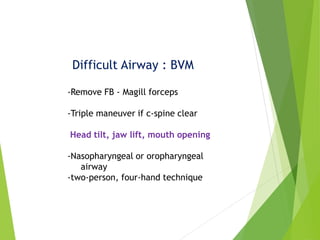
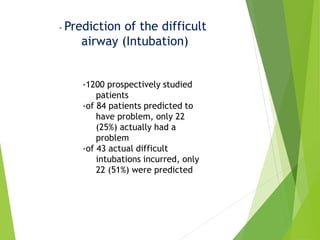
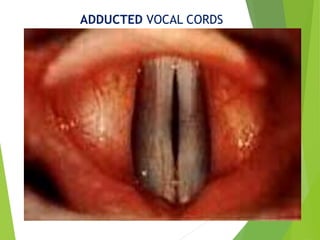
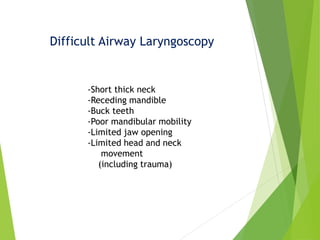
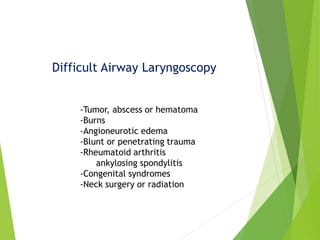
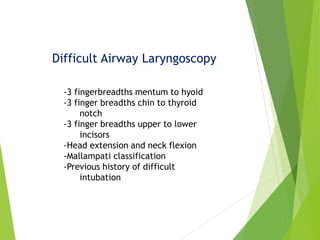
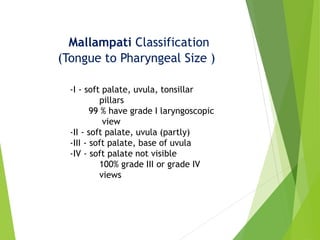
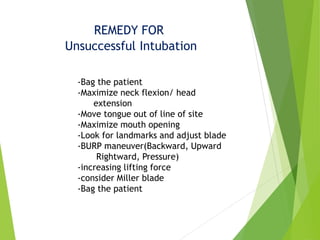
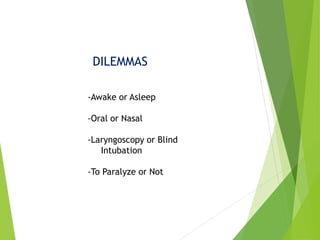
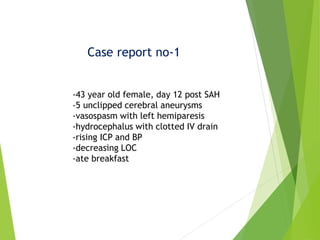
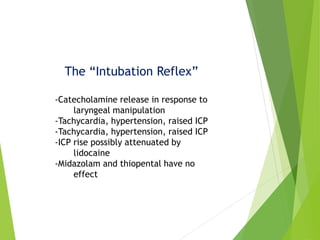
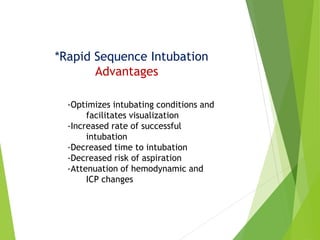
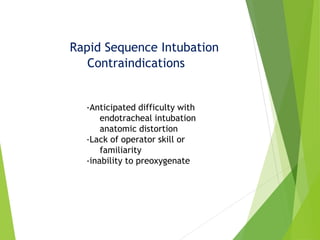
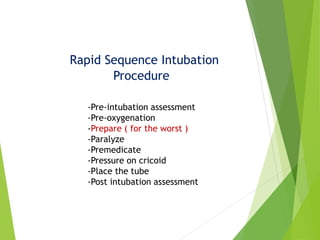
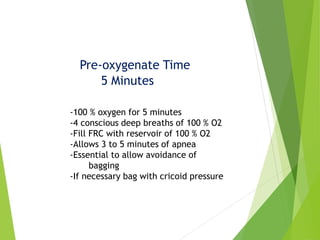
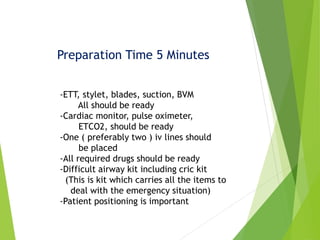
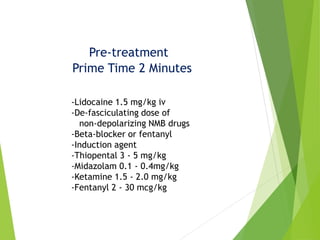
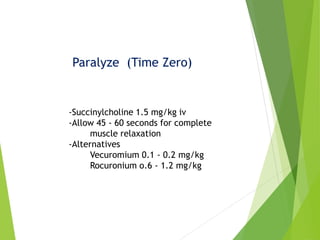
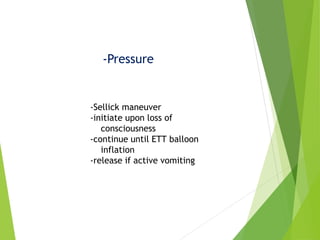
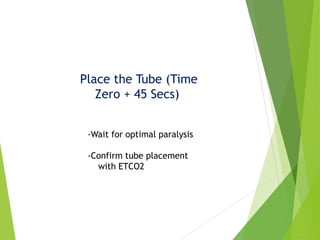
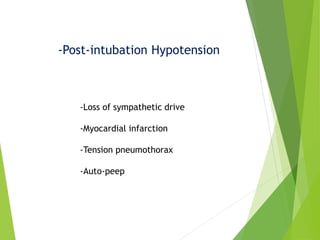
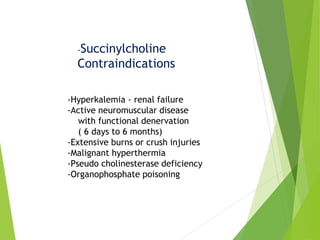
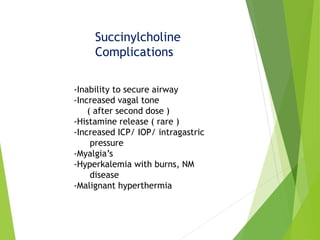
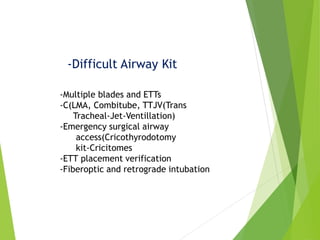
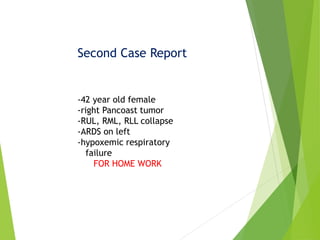
This document discusses various techniques for airway management, with a focus on bag-valve-mask ventilation and endotracheal intubation. It outlines the principles of safe airway assessment and management, including identifying difficult airway factors and developing alternative plans. Rapid sequence intubation is described as the near-simultaneous administration of sedative-hypnotic and neuromuscular blocking drugs to optimize intubation conditions while minimizing aspiration risk. Key steps like pre-oxygenation, drug administration and cricoid pressure are emphasized. Difficult airway scenarios and emergency surgical airway techniques are also addressed.