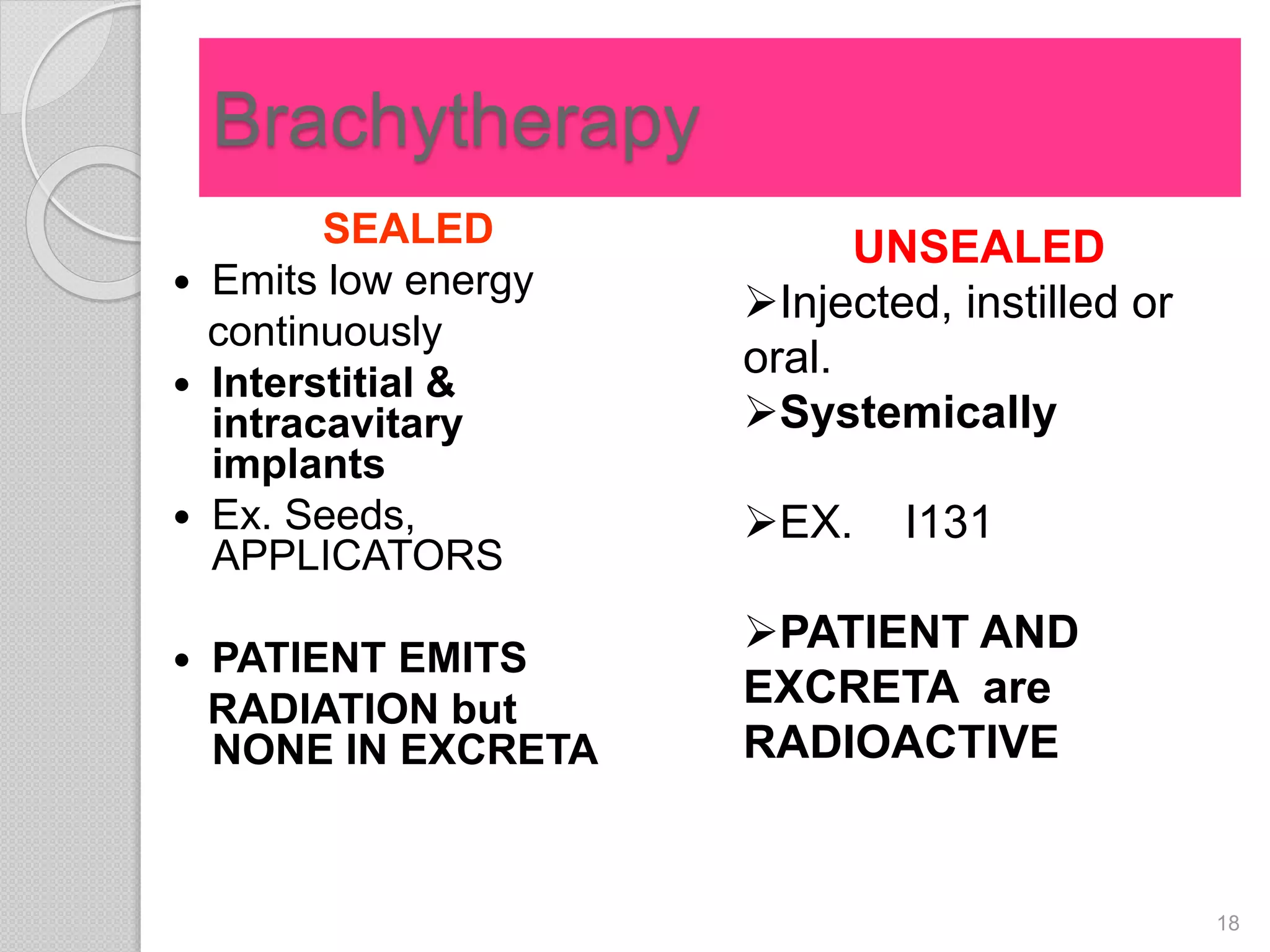
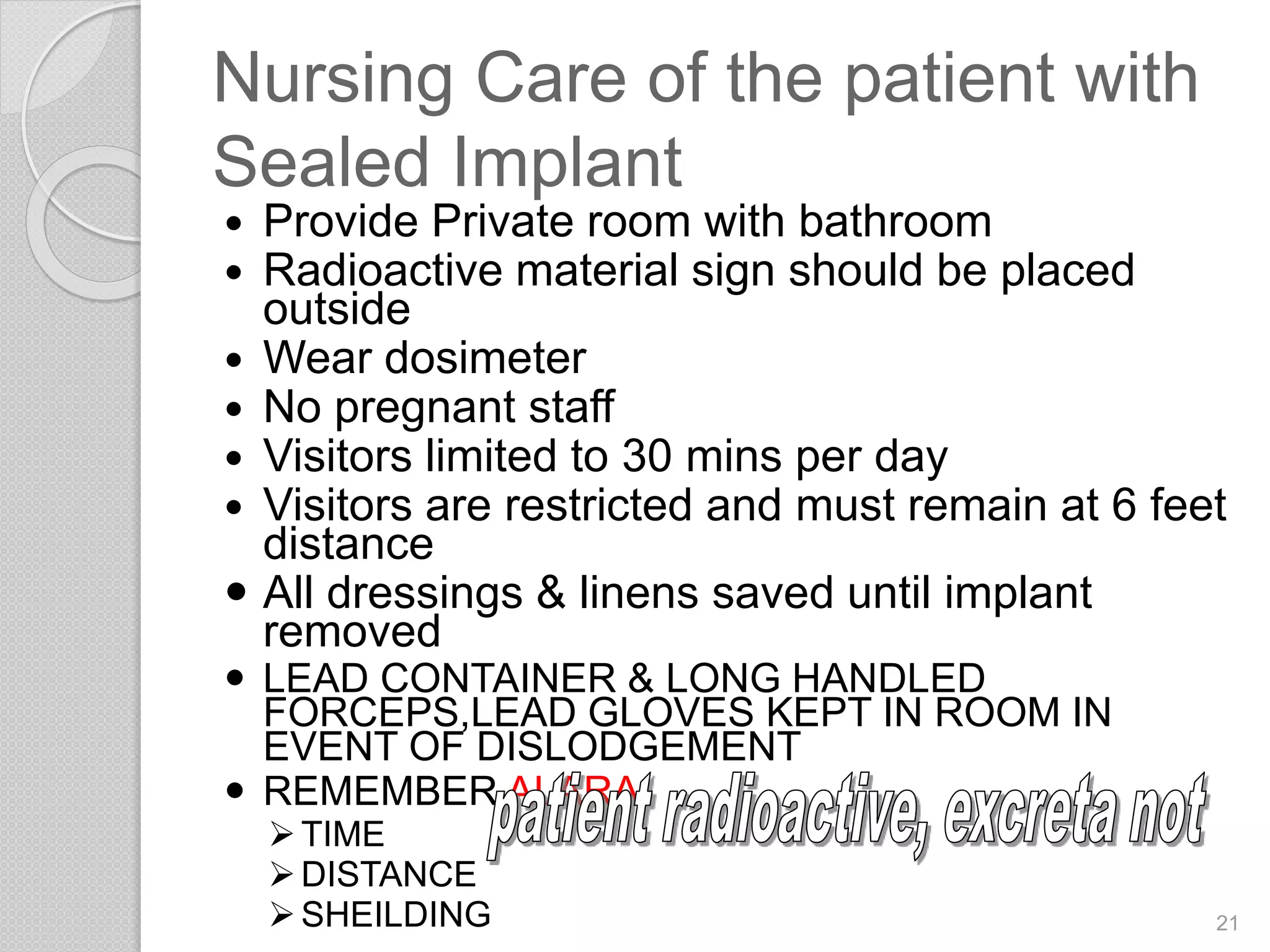
The document provides an introduction to radiation oncology nursing, describing the different types of radiation therapy including external beam radiation and brachytherapy, the goals and mechanisms of radiotherapy, nursing care of patients receiving radiation including symptom management, and side effects of radiation treatment. Radiation oncology nurses play an important role in caring for cancer patients undergoing radiotherapy by ensuring radiation safety, managing side effects, and providing education to patients.