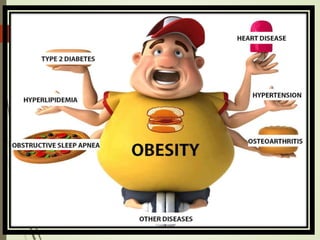
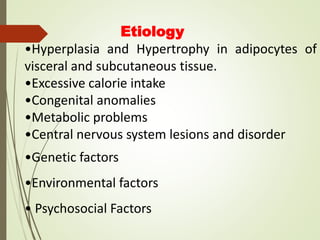
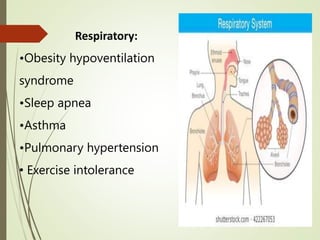
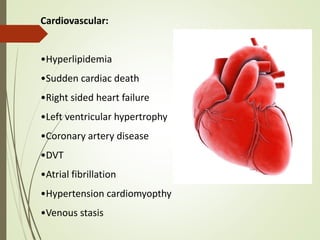
This document discusses obesity, including its definition, classification, causes, health risks, diagnosis, and management. Obesity is defined as excess body fat accumulation that negatively impacts health, and is classified using body mass index (BMI), waist circumference, and waist-to-hip ratio. Causes include genetic, environmental, and behavioral factors. Health risks associated with obesity include increased risk of diabetes, cardiovascular disease, respiratory issues, cancers, and mental health conditions. Treatment involves lifestyle modifications focusing on diet and exercise, as well as potential medication options to help with weight loss.



![3.Anthropometric Measurements:
4. Physical examination:
5. Functional status:
•Ability to perform basic and instrumental
activities
•Performance test. [e.g. timed walk test]](https://image.slidesharecdn.com/mathew-201129141604/85/NUTRITIONAL-PROBLEMS-OBESITY-19-320.jpg)
![NURSING AND COLLABORATIVE
MANAGEMENT:
Nursing assessment :
History on admission
Minimum Data Set [MDS].
Outcome and Assessment information
Set [OASIS]
Physical examination
Nutritional assessment
Anthropometric measurement .](https://image.slidesharecdn.com/mathew-201129141604/85/NUTRITIONAL-PROBLEMS-OBESITY-25-320.jpg)
![OBESITY
Definition:
obesity is a medical condition in which excess body
fat has accumulated to the extent that it may have a
negative effect on health.
Classification of Body weight and obesity:
•Body mass index[BMI]
•Waist to hip ratio[WHR]
•Waist circumference
•Body shape](https://image.slidesharecdn.com/mathew-201129141604/85/NUTRITIONAL-PROBLEMS-OBESITY-41-320.jpg)
![Body mass index:
BMI is calculated by dividing a person’s weight by the square of
meters
BMI = Wt in kg / (Height in meter]2](https://image.slidesharecdn.com/mathew-201129141604/85/NUTRITIONAL-PROBLEMS-OBESITY-42-320.jpg)
![Waist circumference:
Health risk increase if the waist circumference greater than 40
inches in men and greater than 35 inches in women.
Waist to hip ratio:[WHR]
The ratio is calculated by using the waist
measurement divided by the hip measurement. A WHR
less than 0.8 is optimal and A WHR greater than o.8
indicates more truncal fat.](https://image.slidesharecdn.com/mathew-201129141604/85/NUTRITIONAL-PROBLEMS-OBESITY-43-320.jpg)

![Reproductive:[Women]
•Menstrual irregularities
•Infertility
•Gestational diabetes
Reproductive :[Men]
•Hypogonadism
•Gynecomastia
•Sexual dysfunction](https://image.slidesharecdn.com/mathew-201129141604/85/NUTRITIONAL-PROBLEMS-OBESITY-47-320.jpg)
![Gastrointestinal
•Nonalcoholic steatohepatitis
•Gallstones
•Gastro esophageal reflux disease
Genitourinary
•Kidney cancer
•Chronic kidney disease
•Stress incontinence
Cancer
Esophagus, pancreas, thyroid, colorectal, and
gallbladder cancer[both gender]
Endometrial, breast, and ovarian cancer[women]](https://image.slidesharecdn.com/mathew-201129141604/85/NUTRITIONAL-PROBLEMS-OBESITY-49-320.jpg)
![Serotonin Agonist:
Lorcaserin is a selective serotonin agonist
Phentermine and Topiramate: [Qsymia]
Qsymia is a combination of two drugs ,
phentermine and topiramate. In over weight patients
, phentermine suppresses appetite and topiramate
induces a sense of fullness.](https://image.slidesharecdn.com/mathew-201129141604/85/NUTRITIONAL-PROBLEMS-OBESITY-52-320.jpg)
![Elimination: History of constipation
Activity exercise: History about physical activity, drowsiness,
orthopnea and dyspnea on exertion.
Body mass index >30kg/m2, waist circumference
women>35.6inch[89cm], man >40inch[102cm]
Planning:
Modify eating pattern
Participate in a regular activity program
Achieve and maintain weight loss to a specified level
Minimize or prevent health problems related to obesity](https://image.slidesharecdn.com/mathew-201129141604/85/NUTRITIONAL-PROBLEMS-OBESITY-55-320.jpg)
![Nursing implementation:
1.Successful weight loss , which requires a short term energy deficit
2. successful weight control which requires long term behavior
changes
Nutritional therapy:
Calorie restricted weight reduction diet to be
advised.[1200 calorie per day]
a diet that includes adequate amount of fruits, and
vegetable and meet vitamin A and vitamin C
requirements.](https://image.slidesharecdn.com/mathew-201129141604/85/NUTRITIONAL-PROBLEMS-OBESITY-56-320.jpg)
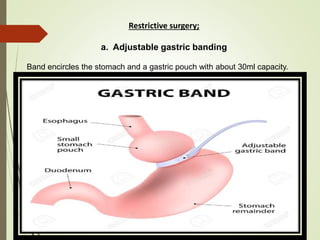
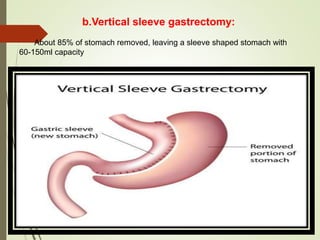
![BARIATRIC SURGERY
Surgery on the stomach and/or intestines to help a person
with extreme obesity loss weight. Bariatric surgery is an option
for people who have a body mass index above 40.
Criteria for bariatric surgery:
•Criteria guidelines for bariatric surgery include having a BMI
of 40kg/m2 or 35kg/m2 with one or more obesity related
medical complications.[e. g. hyper tension, DM type 2, heart
failure] .](https://image.slidesharecdn.com/mathew-201129141604/85/NUTRITIONAL-PROBLEMS-OBESITY-59-320.jpg)