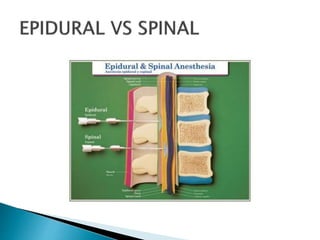
This document discusses the history and practice of anaesthesia. It begins by defining anaesthesia and its historical origins in 1846 when William Morton first demonstrated ether anaesthesia. It then covers levels of anaesthesia including general, local, and regional anaesthesia. The stages of general anaesthesia and types of regional anaesthesia like epidural and spinal blocks are explained. Common agents used in local and regional anaesthesia are named. Complications are also briefly mentioned.