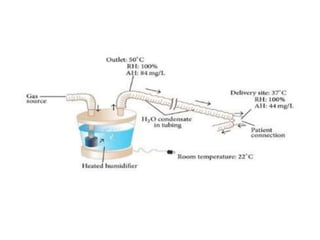
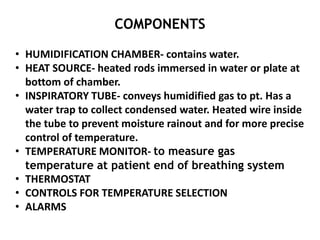
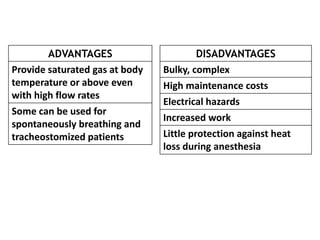
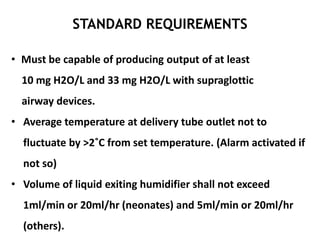
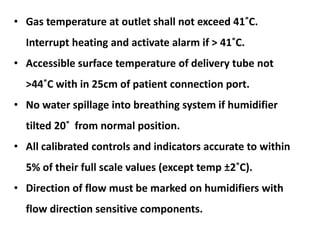
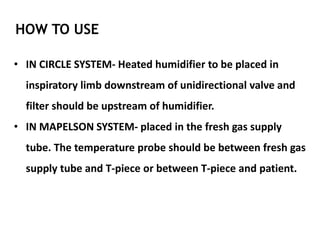
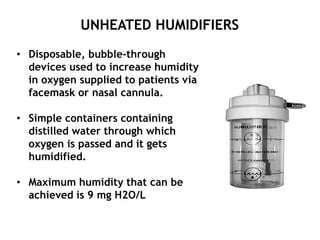
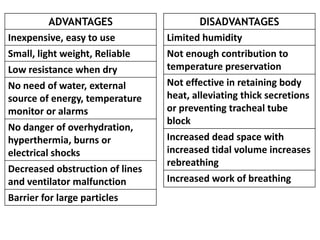
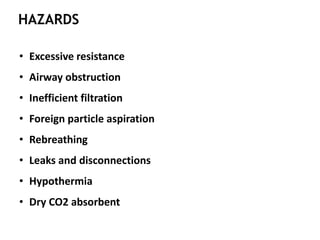
This document discusses humidifiers and humidity in the context of anesthesia. It defines key humidity terms and explains that medical gases are delivered dry in order to prevent equipment issues, but this can damage the respiratory tract. Humidifiers add moisture to gases and are classified as active, using an external heat/water source, or passive, utilizing patient temperature/hydration. Active humidifiers immediately humidify gas while passive HMEs conserve some exhaled moisture and heat. The document discusses various humidifier types, their uses, standards, and hazards.