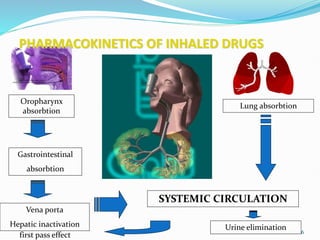
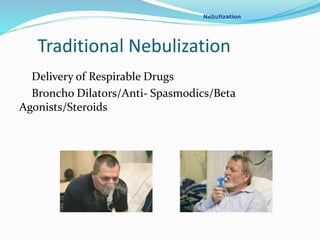
A nebulizer uses oxygen, compressed air, or ultrasonic power to break up medical solutions into fine aerosol droplets that can be directly inhaled. There are several types of nebulizers including jet, ultrasonic wave, soft mist inhaler, and human-powered. The document discusses the history, components, mechanisms, indications, and factors affecting various nebulizer technologies. Nebulizers provide targeted drug delivery to the lungs with rapid onset and fewer systemic side effects compared to other administration methods.



![ Soft Mist Inhaler
Respimat Soft Mist Inhaler in 1997. This new
technology provides a metered dose to the user, as the
liquid bottom of the inhaler is rotated clockwise 180
degrees by hand, adding a build up tension into a
spring around the flexible liquid container. When the
user activates the bottom of the inhaler, the energy
from the spring is released and imposes pressure on
the flexible liquid container, causing liquid to spray
out of 2 nozzles, thus forming a soft mist to be
inhaled. The device features no gas propellant and no
need for battery/power to operate. The average droplet
size in the mist was measured to a somewhat
disappointing 5.8 micrometers, which could indicate
some potential efficiency problems for the inhaled
medicine to reach the lungs.]](https://image.slidesharecdn.com/nebulization-240223123517-8b76b6cd/85/NEBULIZATION-pptx-anesthesia-pediatric-21-320.jpg)
![ Human Powered Nebulizer (HPN)
The most recent innovation in nebulizer technology .
The human-powered nebulizer (HPN) is designed to
provide relief to patients suffering from respiratory
diseases such as asthma, TB, or chronic obstructive
pulmonary disease in areas with limited access to
electricity. Invented in 2009 by a team of doctors from
Marquette University, HPN uses a bicycle frame and
pedals—each connected to a piston and some
tubing—to turn liquid medicine into mist that flows
directly into a patient's lungs through an attached
mouthpiece. Commercial nebulizers typically use an
electric compressor to maintain their rate of airflow,
but with HPN, healthcare workers achieve the same
goal by pedaling the equivalent of 8 miles per hour.[7]](https://image.slidesharecdn.com/nebulization-240223123517-8b76b6cd/85/NEBULIZATION-pptx-anesthesia-pediatric-22-320.jpg)