1) Suctioning refers to clearing secretions from the airways of patients unable to do so themselves, such as those with artificial airways like endotracheal or tracheostomy tubes. It is indicated for patients who cannot cough effectively.
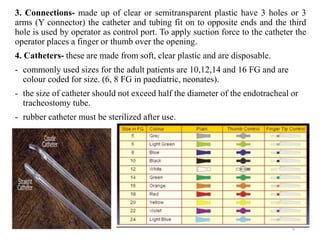
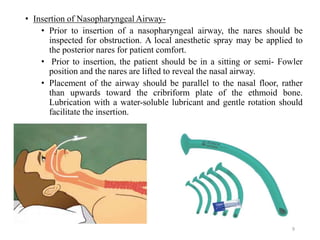
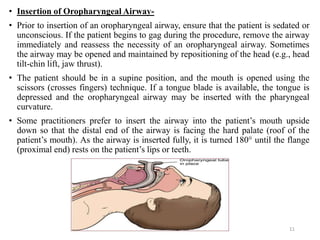
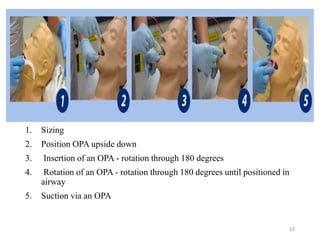
2) There are various suction equipment including pumps, tubing, connectors, and catheters that are used through different entry modes like nasopharyngeal, oropharyngeal, or through artificial airways. Proper technique and sizing is important to avoid hazards.
3) Hazards of suctioning include infection, mucosal trauma, hypoxia, and increased intracranial pressure, so pre-oxygenation and careful technique