This document discusses the management of fulminant ulcerative colitis, a potentially life-threatening condition. It describes:
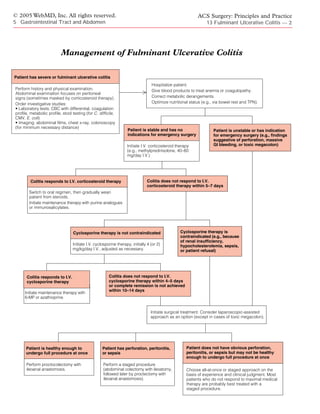
1) Initial evaluation involves a thorough history, physical exam, and tests like bloodwork and imaging to assess severity and rule out complications.
2) Medical management begins with IV corticosteroids, and if that fails within 5-7 days, cyclosporine therapy is considered.
3) Surgery is indicated if medical therapies are not effective or complications develop. The staged or "all-at-once" surgical approach depends on the patient's condition and experience of the surgical team.
![© 2005 WebMD, Inc. All rights reserved. ACS Surgery: Principles and Practice
5 Gastrointestinal Tract and Abdomen 13 Fulminant Ulcerative Colitis — 1
13 FULMINANT ULCERATIVE COLITIS
Roger D. Hurst, M.D., F.A.C.S., F.R.C.S.Ed., and Fabrizio Michelassi, M.D., F.A.C.S.
Fulminant ulcerative colitis is a potentially life-threatening dis- be hospitalized for aggressive resuscitation while clinical assessment
order that must be expertly managed if optimal outcomes are and treatment are being initiated.11
to be achieved. This condition was once associated with a very
high mortality,1 but medical and surgical treatments have im-
proved dramatically, to the point where the mortality associat- Clinical Evaluation
ed with fulminant ulcerative colitis is now lower than 3%.2,3 When a patient is admitted with
Optimal management depends on close coordination between severe or fulminant ulcerative colitis, a
medical and surgical therapy, and multidisciplinary strategies complete history and a thorough physi-
are essential. cal examination are required. The
abdominal examination should focus
on signs of peritoneal irritation that
Classification may suggest perforation or abscess for-
The most commonly applied system of classifying the severity mation. Any patient admitted with severe
of ulcerative colitis has been the one devised by Truelove and ulcerative colitis may have already receiv-
Witts, who identified clinical parameters by which colitis could be ed substantial doses of corticosteroids, which can mask the phys-
categorized as mild, moderate, or severe.4 The Truelove-Witts clas- ical findings of peritonitis.
sification does not, however, specify a unique category for fulmi-
nant disease. Accordingly, Hanauer modified this classification
scheme to include a category for fulminant colitis [see Table 1].5 Investigative Studies
Unfortunately, there is no universally agreed upon distinction be-
LABORATORY TESTS
tween severe ulcerative colitis and fulminant ulcerative colitis.6
Some authors use the terms severe and fulminant interchangeably, Initial laboratory studies should include a complete blood count
whereas others, concerned about the lack of a clear distinction be- with differential, a coagulation profile, and a complete metabolic
tween the two, recommend that the term fulminant ulcerative col- profile with assessment of nutritional parameters (e.g., serum albu-
itis be avoided altogether.7 This latter recommendation has not min concentration). Multiple stool specimens should be sent to be
been widely followed: the term fulminant ulcerative colitis remains tested for Clostridium difficile, cytomegalovirus, and Escherichia coli
an established component of the medical vernacular, the absence 0157:H7.12,13 It is important to rule out the presence of oppor-
of a clear definition notwithstanding.8-10 tunistic infections, particularly with C. difficile, even in patients with
Fulminant ulcerative colitis is certainly a severe condition that is an established diagnosis of ulcerative colitis; superinfection with
associated with systemic deterioration related to progressive ulcera- C. difficile is common in such patients.
tive colitis. Most authorities would agree that a flare of ulcerative col-
IMAGING
itis can be considered fulminant if it is associated with one or more
of the following: high fever, tachycardia, profound anemia necessi- Abdominal films and an upright chest x-ray should be obtained
tating blood transfusion, dehydration, low urine output, abdominal to look for colonic distention (indicative of toxic megacolon) and
tenderness with distention, profound leukocytosis with a left shift, free intraperitoneal air (indicative of perforation).
severe malaise, or prostration. Patients with these symptoms should Endoscopic evaluation of the colon and rectum in the presence
Table 1—Criteria for Evaluating Severity of Ulcerative Colitis
Variable Mild Disease Severe Disease Fulminant Disease
Stools < 4/day > 6/day > 10/day
Blood in stool Intermittent Frequent Continuous
Temperature Normal > 37.5° C > 37.5° C
Pulse Normal > 90 beats/min > 90 beats/min
Hemoglobin Normal < 75% of normal Transfusion required
Erythrocyte sedimentation rate ≤ 30 mm/hr > 30 mm/hr > 30 mm/hr
Colonic features on radiography __ Air, edematous wall, thumbprinting Dilatation
Clinical signs __ Abdominal tenderness Abdominal distention and tenderness](https://image.slidesharecdn.com/acs0513-fulminantulcerativecolitis-2005-100726063323-phpapp02/85/Acs0513-Fulminant-Ulcerative-Colitis-2005-1-320.jpg)
![© 2005 WebMD, Inc. All rights reserved. ACS Surgery: Principles and Practice
5 Gastrointestinal Tract and Abdomen 13 Fulminant Ulcerative Colitis — 3
of fulminant ulcerative colitis is a controversial measure.14-16 Un- flares of ulcerative colitis reported no significant difference in out-
doubtedly, colonoscopy with biopsy can provide useful diagnostic come between those who were managed with total parenteral
information in this setting, and numerous reports indicate that in nutrition (TPN) and bowel rest and those who received enteral
experienced hands, colonoscopy poses little risk to patients with nutrition. This study, however, included patients with colitis of
severe colitis.14,15 In general, however, it is recommended that en- varying degrees of severity, and apparently, only a small number
doscopic examination proceed no further than the minimum dis- of them had fulminant ulcerative colitis.19 A subsequent study
tance necessary to confirm severe colitis. If an endoscopic exami- found that bowel rest and TPN did have a potential clinical
nation is to be performed, insufflation of air must be minimized; advantage in patients with fulminant ulcerative colitis.18 The most
overdistention of the colon may lead to perforation or the develop- common approach to nutritional management of these patients is
ment of megacolon. In addition to diagnostic information, en- first to place them on bowel rest with hyperalimentation, then to
doscopy can provide useful prognostic information. In one study, initiate oral feeding once the symptoms of the fulminant attack
the presence of deep, extensive colonic ulcerations indicated a low begin to be alleviated. Whether patients are being maintained on
probability for successful medical treatment of fulminant ulcera- bowel rest or are receiving oral feedings, adequate nutritional
tive colitis: fewer than 10% of patients with such ulcerations res- support must always be ensured. Hence, TPN, if employed,
ponded to medical measures.14 Thus, an endoscopic finding of should be maintained until the patient is receiving and tolerating
deep ulcers [see Figure 1] may facilitate the decision to proceed full enteral feedings.
with early operative treatment if medical therapy does not lead to
MEDICAL THERAPY
rapid and significant improvement.
The standard medical approach to
fulminant ulcerative colitis involves
Management induction of remission by means of
I.V. corticosteroid therapy, followed
GENERAL CARE
by long-term maintenance treatment
All patients with fulminant ulcerative (in the form of purine analogues) once
colitis should be hospitalized. Blood remission has been achieved. If treat-
products should be administered to ment with steroids fails to induce
treat significant anemia or coagulopa- remission, I.V. cyclosporine therapy is
thy. Metabolic derangements should be considered.
corrected.17 Patients with a perforation
or massive lower GI hemorrhage are Steroids
taken to the operating room for emergency surgical treatment; For decades, steroid treatment has been the frontline therapy
more stable patients are initially managed with medical therapy. for acute flares of ulcerative colitis. Response rates in cases of ful-
Narcotics, antidiarrheal agents, and other anticholinergic medica- minant ulcerative colitis range from 50% to 60% when the
tions should be avoided because they can precipitate toxic dilation steroids are given over a period of 5 to 10 days.20,21 Methylpre-
of the colon. dnisolone, 40 to 60 mg/day in a continuous I.V. infusion, is a
Bowel rest typically reduces the volume of diarrhea, but common regimen.5,22-24
whether it affects the clinical course of the fulminant colitis The length of time that should be allowed for patients to
remains to be established.18,19 One study of patients with acute respond to I.V. steroid therapy has been a subject of debate. In
1974,Truelove and Jewell recommended urgent operative treat-
ment after 5 days if there is no response to I.V. steroid therapy.25
This 5-day rule has been widely adopted, but more recent expe-
rience suggests that steroids can be safely administered for as
long as 7 to 10 days to allow patients more time to respond.12
Patients who respond to I.V. steroid therapy are switched to
an oral steroid regimen (typically prednisone). It is important,
however, to stress that corticosteroids should never be employ-
ed as long-term maintenance therapy.5,26 The toxic effects of
corticosteroids are related to not only the dosage but also the
duration of treatment. Severe complications are common with
extended use of even modest doses of steroids. Accordingly,
patients should be slowly but completely weaned from steroid
therapy. Because symptomatic colitis recurs in 40% to 50% of
patients who initially respond to I.V. therapy, maintenance ther-
apy with either purine analogues or immunosalicylates should
be instituted.5,20
Unfortunately, corticosteroid dependency is frequently encoun-
tered in patients with ulcerative colitis. Often, the steroid dosage
cannot be tapered without an increase in disease activity and exac-
erbation of symptoms. In such cases, if the patient cannot be
weaned from steroids and switched to purine analogues within 3 to
6 months, surgical consultation is indicated. In addition, if compli-
Figure 1 Sigmoidoscopy demonstrates deep ulcerations cations related to ulcerative colitis or to corticosteroid therapy
in a patient with fulminant ulcerative colitis. develop, the colitis must be treated surgically.](https://image.slidesharecdn.com/acs0513-fulminantulcerativecolitis-2005-100726063323-phpapp02/85/Acs0513-Fulminant-Ulcerative-Colitis-2005-3-320.jpg)
![© 2005 WebMD, Inc. All rights reserved. ACS Surgery: Principles and Practice
5 Gastrointestinal Tract and Abdomen 13 Fulminant Ulcerative Colitis — 4
Cyclosporine
At one time, patients who did not re- Table 2—Indications for Operation in Patients
spond to I.V. steroid treatment were in-
with Fulminant Ulcerative Colitis
variably referred for surgical treatment.
Currently, such patients are most often Inability to tolerate medical treatment
treated with I.V. cyclosporine therapy. Failure to respond to medical treatment
Cyclosporine is an immunosuppressant Inability to be weaned from corticosteroids
macrolide that suppresses the production Presence of complications of ulcerative colitis (e.g., perforation, peritonitis,
progressive signs of sepsis, hemorrhage, and toxic megacolon)
of interleukin-2 by activated T cells
Development of complications related to medical treatment
through a calcineurin-dependent path-
way.27 Originally employed to prevent tissue rejection after trans-
plantation, cyclosporine has become the standard treatment of
steroid-refractory severe ulcerative colitis. received large amounts of corticosteroids may increase the risk of
The first report of the use of cyclosporine to treat ulcerative co- perioperative morbidity and mortality in those who respond to
litis was published in 1984.28 It was not until 10 years later, how- neither steroids nor cyclosporine therapy and thus require opera-
ever, that a randomized, placebo-controlled trial of cyclosporine tive management. At present, however, there is no evidence that
therapy for steroid-refractory ulcerative colitis convincingly patients who do not respond to cyclosporine therapy are at
demonstrated the effectiveness of cyclosporine in this setting.29 In increased risk for perioperative complications; such therapy does
this trial, patients with steroid-refractory ulcerative colitis who not appear to compromise surgical results.42
received cyclosporine (4 mg/kg) had an 82% response rate, com-
SURGICAL THERAPY
pared with a 0% response rate in those treated with continued I.V.
steroid therapy alone. Since this initial report, response rates rang-
ing from 56% to 91% have been reported in the medical literature, Indications
confirming cyclosporine as a major advance in the treatment of Indications for surgical treatment of
severe and fulminant ulcerative colitis.30-32 fulminant ulcerative colitis have been
The beneficial effects of cyclosporine therapy are not always established [see Table 2]. One such indi-
durable: as many as 60% of patients experience recurrence of disease cation, of course, is the exhaustion of
after initial cyclosporine-induced remission.33 Fortunately, recur- options for appropriate medical treat-
rence rates can be substantially lowered by means of maintenance ment. Because most patients with fulmi-
therapy with 6-mercaptopurine (6-MP) or azathioprine.With appro- nant ulcerative colitis respond to aggres-
priate maintenance therapy, the rate of early recurrence of symptoms sive medical therapy, such treatment is
after successful I.V. cyclosporine treatment may be reduced to levels warranted in almost all cases. Care must be exercised, however, not
as low as 22%.31,34 Even if the disease does recur, the initial success to overtreat patients with fulminant ulcerative colitis who are other-
of cyclosporine therapy in aborting the acute phase of the ulcerative wise stable. The immunosuppressive effects of high-dose cortico-
colitis allows patients to recover from the acute illness, so that they steroids and I.V. cyclosporine, along with the debilitation induced by
are in better condition to undergo elective surgical treatment at a lat- prolonged severe disease, can place patients at high risk for periop-
er date if such treatment ultimately proves necessary.This is a major erative complications. Patients who do not show significant improve-
benefit, in that operative management of ulcerative colitis carries a ment in response to I.V. steroid therapy within 5 to 7 days should be
much higher risk of complications when carried out on an urgent ba- started on I.V. cyclosporine therapy or referred for operative treat-
sis than when carried out in an elective setting.18,35,36 ment.12 Those who do not respond to cyclosporine therapy within 4
The major side effects of cyclosporine treatment are renal insuf- days or in whom remission of major symptoms is not achieved with-
ficiency, opportunistic infections, and seizures.The risk of seizures in 2 weeks should be treated surgically. Patients whose symptoms
appears to be highest in patients with hypocholesterolemia. Con- progress during the course of I.V. therapy or who show no sign of
sequently, cyclosporine should not be given to patients with sig- improvement at all should be considered for early surgery. Patients
nificant hypocholesterolemia (serum cholesterol concentration known to have deep longitudinal ulcerations are less likely to
< 100 mg/dl). Hypomagnesemia is commonly seen in patients with respond to I.V. medical therapy and thus may also be referred for
fulminant ulcerative colitis who undergo cyclosporine treatment; early surgery. The decision regarding when to abandon medical
accordingly, serum magnesium levels should be closely followed. therapy for fulminant ulcerative colitis in favor of surgical therapy is
Dosing regimens for cyclosporine vary. The typical starting difficult and requires considerable experience and special expertise.
dosage is 4 mg/kg/day I.V., which is then adjusted to achieve a Accordingly, patients with fulminant ulcerative colitis are best man-
whole-blood level between 150 and 400 ng/ml, as measured by aged in a center specializing in inflammatory bowel disease.
high-power liquid chromatography or radioimmunoassay.37,38 Patients with perforation or severe GI bleeding require urgent
Whole-blood levels as high as 800 ng/ml are considered acceptable surgical treatment.43 The debilitation resulting from the disease,
by some investigators.29 If the patient shows no improvement with- coupled with the immunosuppression resulting from intensive
in 4 to 5 days or if complete remission is not achieved by 10 to 14 medical therapy, can mask the signs and symptoms of sepsis and
days, surgical treatment is advised.12 Most of the side effects of peritonitis associated with perforation. Perioperative mortality in
cyclosporine therapy are dose dependent. Several studies have cases of fulminant colitis is as much as 10 times higher when per-
shown that an initial dosage of 2 mg/kg/day I.V. can also be effec- foration occurs than when it does not.44 For this reason, patients
tive in achieving remission.39-41 Some physicians prefer to begin at with high fever, marked leukocytosis, and persistent tachycardia
this lower dosage and then increase it as necessary on the basis of should be referred for early surgery, regardless of whether other
the measured cyclosporine levels. indications of perforation or peritonitis are noted.
Concerns have been raised about the possibility that prolonging Toxic megacolon, though an uncommon complication of severe
medical therapy in patients with severe colitis who have already ulcerative colitis, is important in that it is associated with impend-](https://image.slidesharecdn.com/acs0513-fulminantulcerativecolitis-2005-100726063323-phpapp02/85/Acs0513-Fulminant-Ulcerative-Colitis-2005-4-320.jpg)
![© 2005 WebMD, Inc. All rights reserved. ACS Surgery: Principles and Practice
5 Gastrointestinal Tract and Abdomen 13 Fulminant Ulcerative Colitis — 5
ing colonic perforation and therefore must be watched for and weaned from immunosuppressive agents, and to achieve improved
aggressively managed if present. Two specific conditions must be nutritional status. Although the remaining rectal stump continues
satisfied to establish the diagnosis of toxic megacolon.45 First, to be affected by ulcerative colitis, the fecal diversion greatly dimin-
there must be colonic dilatation; second, the patient must be in a ishes disease activity, so that almost all patients can be completely
toxic state. Patients with mild symptoms of ulcerative colitis may weaned from steroids and other immunosuppressive medications.
experience a degree of colonic dilatation, perhaps in conjunction It is then possible to perform the proctectomy with ileoanal anasto-
with colonic ileus. This condition is distinctly different from and mosis in more controlled conditions.
considerably less worrisome than toxic megacolon. Patients ad- The exact circumstances in which it is best to follow a staged ap-
mitted to the hospital with fulminant ulcerative colitis will, by def- proach have not been clearly defined. It is universally accepted that a
inition, exhibit some degree of toxicity. Colonic dilatation in these staged procedure is mandatory in patients with perforation, peritoni-
patients is a very worrisome phenomenon, in that it completes the tis, or sepsis, but beyond this point, there is no clear consensus.The
picture of toxic megacolon. Accordingly, in all patients with fulmi- studies published to date have been inconclusive on this issue: either
nant ulcerative colitis, an abdominal x-ray should be obtained to they included only a small number of patients, they did not clearly
look for colonic dilatation. Those in whom abdominal distention define what constituted fulminant colitis, or they did not directly
develops or who experience a sudden decrease in the number of compare the results of the two alternative strategies (i.e., staged
bowel movements without signs of significant clinical improvement colectomy and immediate ileoanal anastomosis). A 1995 study re-
should also be assessed for colonic dilatation and toxic megacolon. ported excellent long-term results and acceptable short-term mor-
In patients with toxic megacolon who are otherwise stable, con- bidity in 12 patients undergoing immediate restorative proctoco-
servative management, consisting of elimination of narcotics and an- lectomy with ileal pouch–anal anastomosis (IPAA) for fulminant
ticholinergic agents, may be briefly tried. Changes in patient position colitis.48 These 12 patients, however, represented an extraordinarily
may be tried as well: moving the patient from side to side, from small percentage of the total number of ileoanal procedures per-
supine to prone, and into the knee-elbow prone position is thought formed by the authors. In addition, this study used a somewhat lib-
to facilitate expulsion of colonic gas.46 Patients with toxic megacolon eral definition of fulminant colitis and thus might have included a
should be kept on a nihil per os (NPO) regimen, and broad-spec- number of cases that would not have qualified as fulminant colitis—
trum I.V. antibiotics should be given. Endoscopic decompression is or, possibly, even as severe colitis—according to the criteria cited ear-
to be avoided. Blind placement of rectal tubes is ineffective and may lier [see Table 1]. Finally, the study provided no data on the experi-
be harmful. Patients who do not rapidly respond to conservative ence of patients undergoing a staged procedure for the management
management and those who show signs of peritonitis or are other- of severe or fulminant colitis.
wise unstable require urgent surgical treatment.47 A 1994 study also reported excellent long-term results and ex-
ceptionally low perioperative morbidity in 20 patients undergoing
Preparation for Operation restorative proctocolectomy with IPAA for urgent treatment of ul-
With patients who are stable but are not responding to med- cerative colitis.49 Another study from the same year, however, re-
ical therapy, there may be time for preoperative preparation. ported a 41% anastomotic leakage rate in 12 patients also under-
Patients who are not on NPO status should be maintained on going an urgent ileoanal procedure for ulcerative colitis, compared
clear liquids, then kept on an NPO regimen for 6 to 8 hours with an 11% leakage rate in patients undergoing ileoanal anasto-
before operation. On occasion, a patient may be able to tolerate mosis under more controlled conditions.50 On the basis of these
mild bowel preparation with either polyethylene glycol or Fleet results, the authors counseled against ileoanal anastomosis in the
Phospho-soda (Fleet Pharmaceuticals, Lynchburg, Virginia). urgent setting. A later study also noted a higher incidence of anas-
Any bowel preparations that are used need be employed only tomotic leakage (36%) in patients undergoing urgent ileoanal
until bowel movements are free of residue. If time allows, the anastomosis.51 These authors likewise advised against ileoanal
patient should be counseled by an experienced enterostomal anastomosis in the urgent setting.
therapist, and an optimal site for the ostomy should be marked The fact of the matter is that the distinction between severe and
on the abdomen. Prophylactic antibiotics should be given before fulminant ulcerative colitis may be little more than an academic ex-
the the surgical incision is made, and appropriate stress-dose ercise. At one end of the disease spectrum, there is a small subset of
steroids should be administered. patients who have symptoms severe enough to necessitate hospital-
ization yet are healthy enough to undergo a primary ileoanal anasto-
Surgical Strategies mosis without undue risk. At the other end of the spectrum, there is
The operative strategies for treating a subset of severely ill patients with fulminant colitis for whom a
fulminant ulcerative colitis are contro- staged procedure is mandatory.The middle of the spectrum remains
versial. Ultimately, almost all patients something of a gray area. Because specific criteria for quantifying the
end up undergoing a restorative procto- risk have not been defined, the decision whether to follow a staged
colectomy with ileoanal anastomosis [see operative approach ultimately is made on the basis of the experi-
5:33 Procedures for Ulcerative Colitis]. In enced surgeon’s clinical judgment. It has been our experience, how-
most cases, however, the final surgical ever, that the majority of patients who fit the criteria of fulminant col-
goal is achieved in multiple steps. Per- itis [see Table 1] and who do not respond to maximal medical therapy
forming an extensive resection in con- are best managed with a staged approach.
junction with a prolonged and delicate reconstruction in an acute-
ly ill patient is a procedure of questionable safety. Accordingly, Technical Considerations
many surgeons elect first to perform a total abdominal colectomy Surgical exploration is performed via either a midline or a trans-
with an ileostomy, leaving the rectal stump as either a Hartmann verse incision.The abdomen is carefully examined, with particular
pouch or a mucous fistula,43,44 then to perform a restorative proc- attention paid to the small intestine in an effort to detect any signs of
tectomy with ileoanal anastomosis at a later date. This staged ap- Crohn disease.The colon often shows the changes typical of colitis:
proach allows the patient to recover from the acute illness, to be serosal hyperemia, corkscrew vessels, and edema [see Figure 2].](https://image.slidesharecdn.com/acs0513-fulminantulcerativecolitis-2005-100726063323-phpapp02/85/Acs0513-Fulminant-Ulcerative-Colitis-2005-5-320.jpg)
![© 2005 WebMD, Inc. All rights reserved. ACS Surgery: Principles and Practice
5 Gastrointestinal Tract and Abdomen 13 Fulminant Ulcerative Colitis — 6
Figure 2 In a colon affected by fulminant ulcerative colitis, Figure 3 Shown is a Hartmann pouch constructed at the
changes on the serosal aspect are typically subtle. Serosal level of the sacral promontory. TA staple line is reinforced
hyperemia with small corkscrew vessels is present. with interrupted silk Lembert sutures.
Figure 4 Surgical specimen from a patient with fulminant Figure 5 Shown is mobilization of splenic flexure during
ulcerative colitis shows severe ulceration and inflammation. laparoscopic colectomy for fulminant ulcerative colitis.
Colectomy may be performed in the standard fashion, with that will assist the surgeon in locating the appropriate presacral
mesenteric division occurring at a convenient distance from the dissection plane for any future planned proctectomy.
bowel; wide mesenteric resection is not necessary. If a staged To create the Hartmann pouch, the mesenteric and peri-
colectomy is to be performed, the colon is removed, and the rec- colonic fat are removed from the bowel wall for a distance of ap-
tum is left either as a Hartmann pouch or as a mucous fistula. In proximately 2 cm. A transverse anastomosis (TA) stapler loaded
most cases, a Hartmann pouch can safely be created. In the con- with 4.8 mm staples is placed on the prepared bowel and fired to
struction of a Hartmann pouch, it is important that the stump be close the pouch.The bowel is then divided proximal to the staple
of the appropriate length. If the stump is too short, the proctecto- line. The staple line should be closely examined to confirm that
my to be performed in the second stage may prove very difficult; if the staples are closed properly into two rows of well-formed Bs
it is too long, there is an increased risk of complications related to and that individual staples are not cutting into the muscularis
persistent disease in the rectum (e.g., bleeding, discharge, and propria of the bowel.To provide additional protection against de-
tenesmus). Ideally, the Hartmann pouch should be made at the hiscence, the staple line may be oversewn with interrupted Lem-
level of the sacral promontory [see Figure 3]. During the colecto- bert sutures [see Figure 3]. If sutures are employed, they should be
my, the sigmoid branches of the inferior mesenteric artery should carefully placed so that the anterior and posterior serosal surfaces
be divided and the terminal branches of the inferior mesenteric are approximated without undue tension.With a well-construct-
artery preserved.This measure ensures a good blood supply to the ed Hartmann pouch, pelvic drains are unnecessary and may even
remaining rectal stump and helps the Hartmann closure to heal. be harmful, in that they can promote dehiscence if situated close
Preservation of the terminal branches of the inferior mesenteric to the suture line.
artery and the superior rectal artery also simplifies the subsequent In some cases, the colon at the level of the sacral promontory is
proctectomy by keeping the pelvic sympathetic nerves free of sur- affected by deep ulcerations and severe inflammation, to the point
rounding scar tissue and by providing a key anatomic landmark where closure of the Hartmann pouch at this level poses an unac-](https://image.slidesharecdn.com/acs0513-fulminantulcerativecolitis-2005-100726063323-phpapp02/85/Acs0513-Fulminant-Ulcerative-Colitis-2005-6-320.jpg)
![© 2005 WebMD, Inc. All rights reserved. ACS Surgery: Principles and Practice
5 Gastrointestinal Tract and Abdomen 13 Fulminant Ulcerative Colitis — 7
ceptably high risk of dehiscence [see Figure 4]. If the severity of dis- beneficial in reducing the risk of dehiscence of the Hartmann
ease precludes safe closure of the Hartmann pouch, creation of a pouch.
mucous fistula should be considered. A mucous fistula requires a
longer segment of bowel than a Hartmann pouch does and thus is Laparoscopic Approaches
associated with a higher risk of bleeding from the retained seg- Experience has demonstrated that laparoscopic-assisted ap-
ment. In addition, a mucous fistula is unsightly and often gener- proaches to abdominal colectomy can be safely employed in patients
ates a very foul odor. As a compromise approach, some surgeons with ulcerative colitis.52 Mobilization of the colon and division of the
advocate creating a Hartmann pouch of moderate length and mesentery can be accomplished laparoscopically [see Figure 5], with
placing the proximal end of the stump through the fascia at the the specimen being removed through a small Pfannenstiel incision.
lower edge of the midline incision; the end of the stump is then left An end ileostomy can also be fashioned with the aid of inspection
buried in the subcutaneous tissue. The benefit of this approach is through the Pfannenstiel incision. Alternatively, the Pfannenstiel in-
that if dehiscence of the staple line occurs, any ensuing infection cision can be made early in the procedure and used for placement of
is limited to the subcutaneous space and does not result in an a hand port, and the colon can be removed by means of a hand-
intra-abdominal or pelvic abscess. assisted laparoscopic approach.
If attempts to fashion a secure Hartmann closure fail and the Whether a laparoscopic-assisted approach to the management of
remaining rectal stump is too short to be brought out as a mucous fulminate ulcerative colitis possesses any significant clinical advan-
fistula, the proximal rectum should be resected, and closure of the tages remains to be determined. However, a growing body of experi-
Hartmann pouch should be performed just below the peritoneal ence with this approach indicates that in experienced hands, laparo-
reflection. In this situation, closed suction drains should be placed scopic-assisted colectomy is a safe and reasonable alternative that may
deep in the pelvis, and the peritoneum should be closed over the well result in shorter hospital stays and decreased postoperative pain.
rectal stump. Such a short Hartmann pouch, however, will be The laparoscopic-assisted approach may therefore be considered as
more difficult to locate during the subsequent restorative proctec- an option for patients with fulminant ulcerative colitis. Patients with
tomy and ileoanal anastomosis. toxic megacolon, however, should be managed by means of an open
With a staged colectomy, an end ileostomy is created in the surgical approach; the instruments used to grasp the bowel in a la-
standard fashion [see 5:30 Intestinal Stomas], and the abdomen is paroscopic-assisted colectomy are likely to cause perforation of the se-
closed. Placing a rectal tube to drain rectal secretions may be verely thinned walls of the dilated megacolon.
References
1 Banks B, Korelitz B, Zetzel I:The course of non-spe- 14. Carbonnel F, Lavergne A, Lemann M, et al: Colon- 1:1067, 1974
cific ulcerative colitis: review of twenty years experi- oscopy of acute colitis: a safe and reliable tool for as- 26. Sachar DB: Maintenance therapy in ulcerative colitis
ence and late results. Gastroenterology 32:983, 1952 sessment of severity. Dig Dis Sci 39:1550, 1994 and Crohn’s disease. J Clin Gastroenterol 20:117,
2. Daperno M, Sostegni R, Rocca R, et al: Medical 15. Alemayehu G, Jarnerot G: Colonoscopy during an 1995
treatment of severe ulcerative colitis. Aliment Phar- attack of severe ulcerative colitis is a safe procedure 27. Faulds D, Goa KL, Benfield P: Cyclosporin: a re-
macol Ther 16(suppl 4):7, 2002 and of great value in clinical decision making. Am J view of its pharmacodynamic and pharmacokinetic
Gastroenterol 86:187, 1991 properties, and therapeutic use in immunoregulatory
3. Jarnerot G, Rolny P, Sandberg-Gertzen H: Intensive
intravenous treatment of ulcerative colitis. Gastroen- 16. Marion JF, Present DH:The modern medical man- disorders. Drugs 45:953, 1993
terology 89:1005, 1985 agement of acute, severe ulcerative colitis. Eur J Gas- 28. Gupta S, Keshavarzian A, Hodgson HJ: Cyclosporin
troenterol Hepatol 9:831, 1997 in ulcerative colitis. Lancet 2:1277, 1984
4. Truelove SC,Witts LJ: Cortisone in ulcerative colitis:
final report on a therapeutic trial. BMJ 2:1041, 1955 17. Travis SP, Farrant JM, Ricketts C, et al: Predicting 29. Lichtiger S, Present DH, Kornbluth A, et al: Cy-
outcome in severe ulcerative colitis. Gut 38:905, closporine in severe ulcerative colitis refractory to
5. Hanauer SB: Inflammatory bowel disease. N Engl J
1996 steroid therapy. N Engl J Med 330:1841, 1994
Med 334:841, 1996
18. Mikkola KA, Jarvinen HJ: Management of fulminat- 30. Stack WA, Long RG, Hawkey CJ: Short- and long-
6. Ludwig D, Stange EF:Treatment of ulcerative coli- ing ulcerative colitis. Ann Chir Gynaecol 81:37,
tis. Hepatogastroenterology 47:83, 2000 term outcome of patients treated with cyclosporin
1992 for severe acute ulcerative colitis. Aliment Pharmacol
7. Hyde GM, Jewell DP:The management of severe ul- 19. McIntyre PB, Powell-Tuck J, Wood SR, et al: Con- Ther 12:973, 1998
cerative colitis. Aliment Pharmacol Ther 11:419, trolled trial of bowel rest in the treatment of severe 31. Loftus CG, Loftus EV Jr, Sandborn WJ: Cyclosporin
1997 acute colitis. Gut 27:481, 1986 for refractory ulcerative colitis. Gut 52:172, 2003
8. Modigliani R: Medical management of fulminant 20. Kornbluth A, Marion JF, Salomon P, et al: How ef- 32. Santos J, Baudet S, Casellas F, et al: Efficacy of intra-
colitis. Inflamm Bowel Dis 8:129, 2002 fective is current medical therapy for severe ulcera- venous cyclosporine for steroid refractory attacks of
9. Swan NC, Geoghegan JG, O’Donoghue DP, et al: tive and Crohn’s colitis? An analytic review of select- ulcerative colitis. J Clin Gastroenterol 20:285, 1995
Fulminant colitis in inflammatory bowel disease: de- ed trials. J Clin Gastroenterol 20:280, 1995
33. Cohen RD, Stein R, Hanauer SB: Intravenous cy-
tailed pathologic and clinical analysis. Dis Colon 21. Faubion WA Jr, Loftus EV Jr, Harmsen WS, et al: closporin in ulcerative colitis: a five-year experience.
Rectum 41:1511, 1998 The natural history of corticosteroid therapy for in- Am J Gastroenterol 94:1587, 1999
10. Danovitch SH: Fulminant colitis and toxic mega- flammatory bowel disease: a population-based study.
34. Kamm MA: Review article: maintenance of remis-
colon. Gastroenterol Clin North Am 18:73, 1989 Gastroenterology 121:255, 2001
sion in ulcerative colitis. Aliment Pharmacol Ther
11. Han PD, Cohen RD: The medical approach to the 22. Rosenberg W, Ireland A, Jewell DP: High-dose 16(suppl 4):21, 2002
patient with inflammatory bowel disease.The Clini- methylprednisolone in the treatment of active ulcera-
35. Hawley PR: Emergency surgery for ulcerative colitis.
cian’s Guide to Inflammatory Bowel Disease. Licht- tive colitis. J Clin Gastroenterol 12:40, 1990
World J Surg 12:169, 1988
enstein GR, Ed. Slack,Thorofare, New Jersey, 2003 23. Farthing MJ: Severe inflammatory bowel disease:
36. Hurst RD, Finco C, Rubin M, et al: Prospective
12. Chang JC, Cohen RD: Medical management of se- medical management. Dig Dis 21:46, 2003 analysis of perioperative morbidity in one hundred
vere ulcerative colitis. Gastroenterol Clin North Am 24. Wolf JM, Lashner BA: Inflammatory bowel disease: consecutive colectomies for ulcerative colitis. Surgery
33:235, 2004 sorting out the treatment options. Cleve Clin J Med 118:748, 1995
13. Kaufman HS, Kahn AC, Iacobuzio-Donahue C, et 69:621, 2002 37. Stein RB, Hanauer SB: Medical therapy for inflam-
al: Cytomegaloviral enterocolitis: clinical associations 25. Truelove SC, Jewell DP: Intensive intravenous regi- matory bowel disease. Gastroenterol Clin North Am
and outcome. Dis Colon Rectum 42:24, 1999 men for severe attacks of ulcerative colitis. Lancet 28:297, 1999](https://image.slidesharecdn.com/acs0513-fulminantulcerativecolitis-2005-100726063323-phpapp02/85/Acs0513-Fulminant-Ulcerative-Colitis-2005-7-320.jpg)
