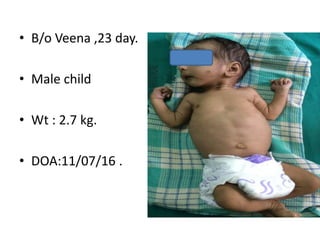
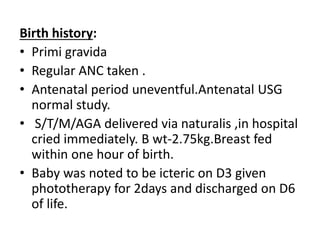
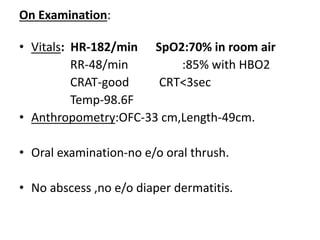
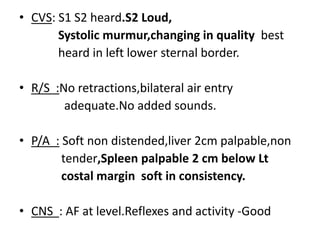
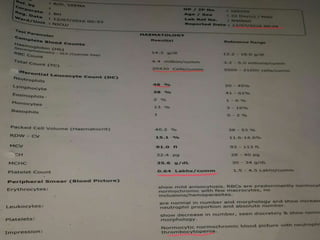
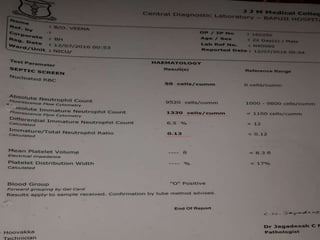
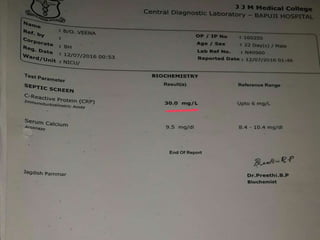
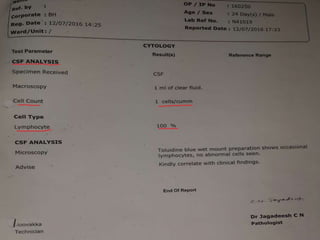
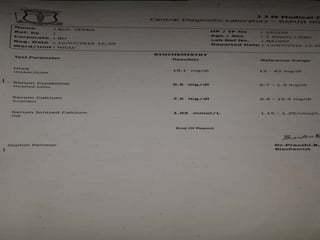
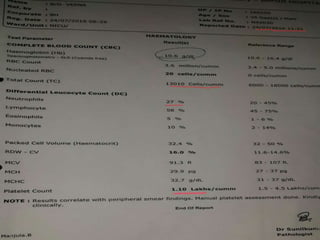
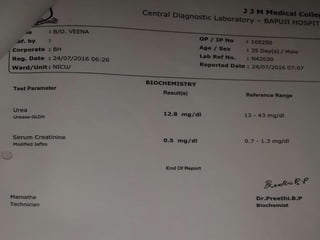
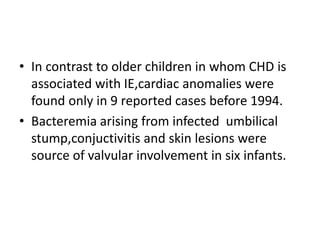
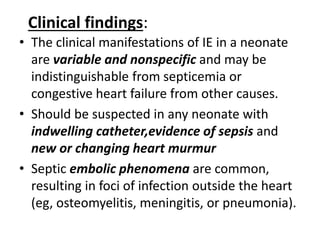
- A 23-day-old male infant presented with fever since 8 days of life and was referred to the hospital for further management. Examination revealed decreased oxygen saturation, tachycardia, a changing murmur, loud heart sounds, and splenomegaly.
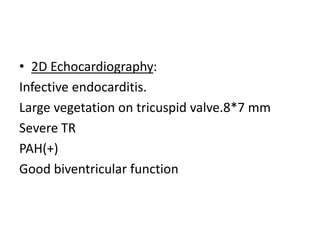
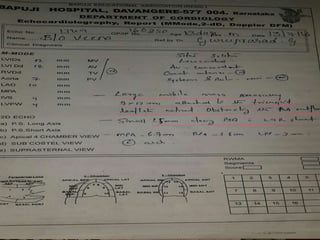
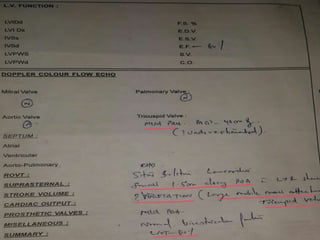
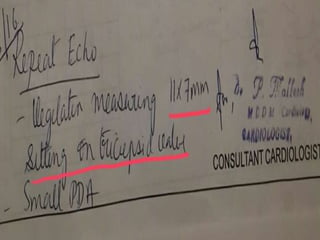
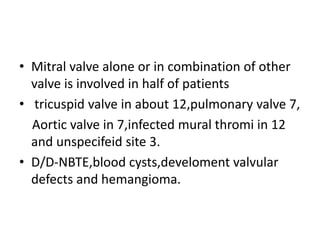
- Echocardiogram showed infective endocarditis with a large vegetation on the tricuspid valve, severe tricuspid regurgitation, and pulmonary artery hypertension.
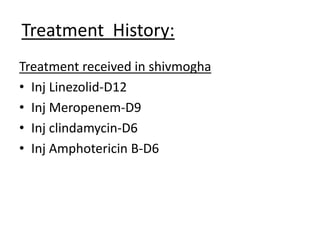
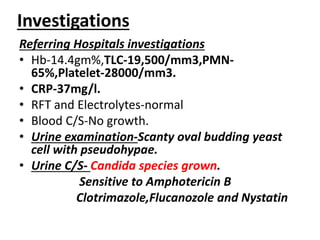
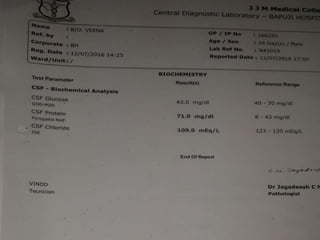
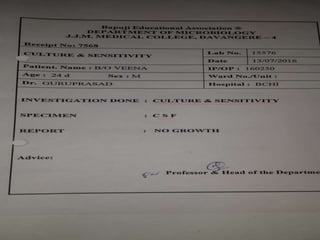
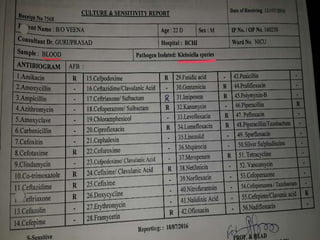
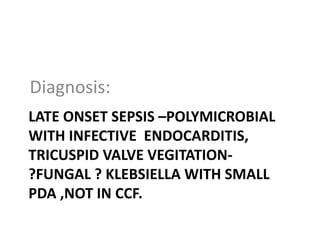
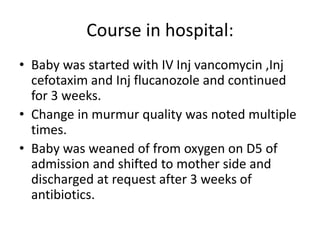
- The diagnosis was late-onset sepsis with possible fungal or Klebsiella infective endocarditis and a small patent ductus arteriosus, but not congestive heart failure. The infant was treated with intravenous antibiotics for 3 weeks and discharged