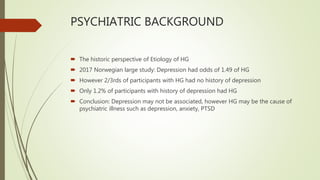
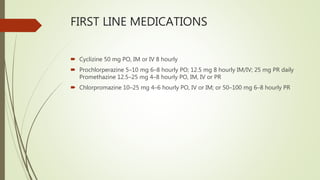
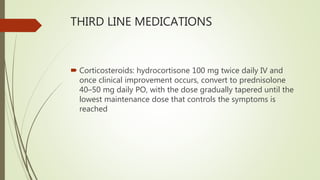
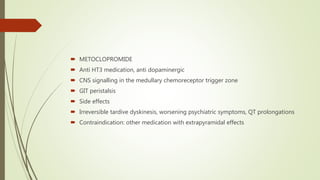
Hyperemesis gravidarum (HG) is a serious condition characterized by excessive vomiting during pregnancy, often necessitating hospitalization due to complications such as dehydration, electrolyte imbalances, and nutritional deficiencies. The document outlines the epidemiology, potential causes including hormonal and genetic factors, clinical diagnosis, and management options for HG, emphasizing the importance of supportive care and antiemetic medications. Complications can affect both maternal and fetal health, highlighting the psychosocial impacts and potential for serious medical issues.