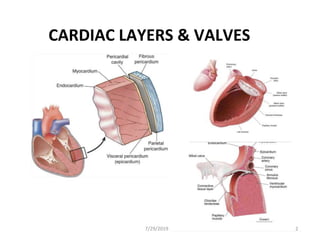
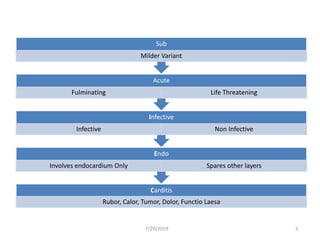
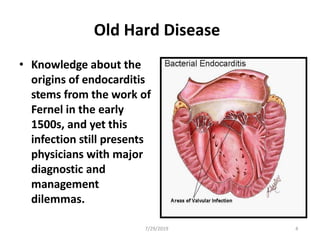
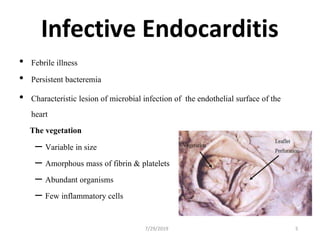
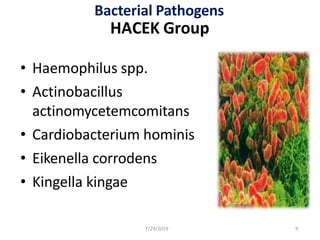
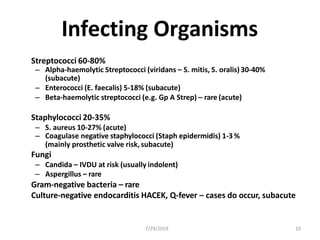
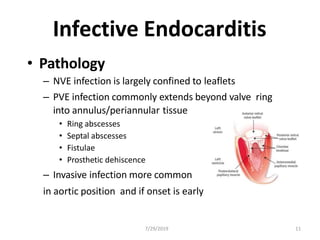
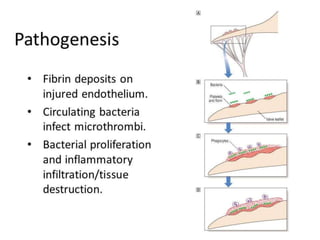
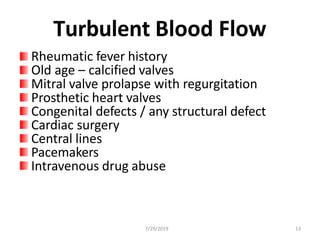
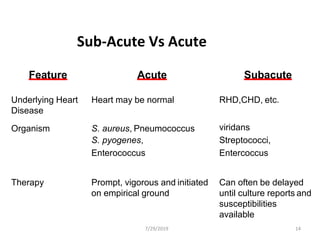
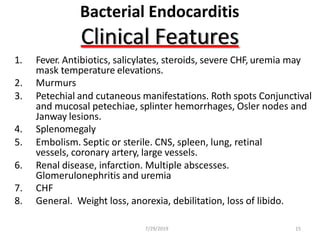
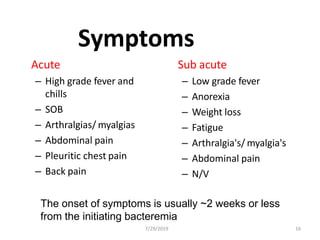
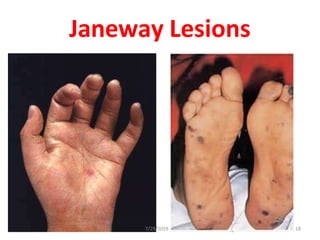
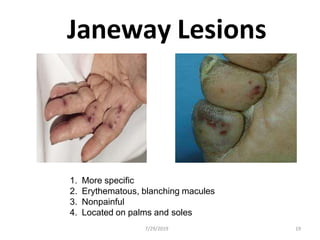
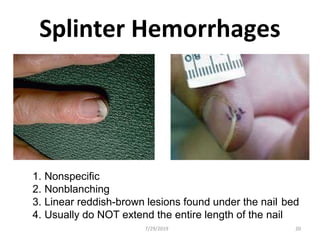
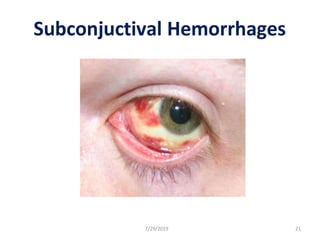
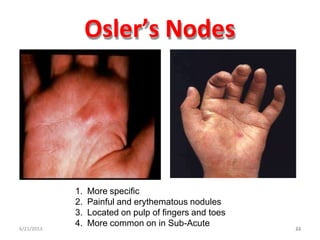
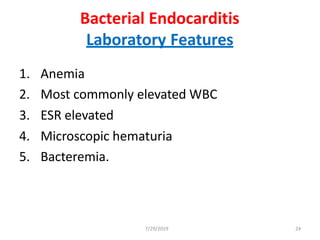
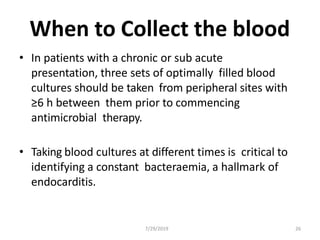
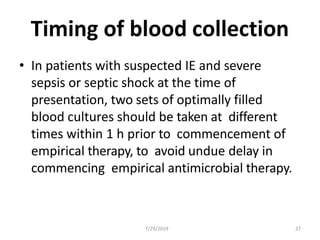
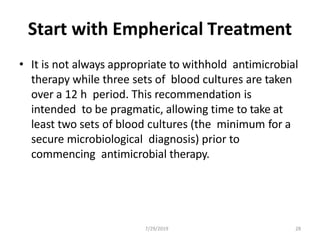
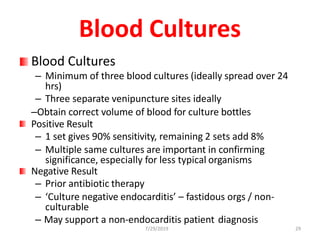
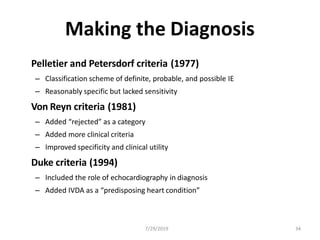
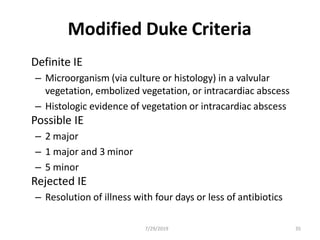
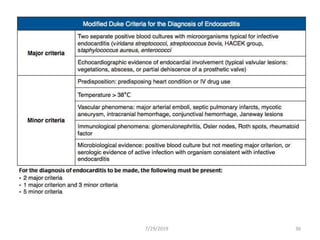
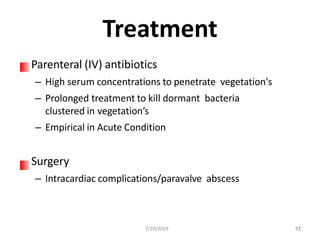
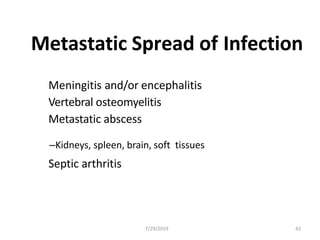
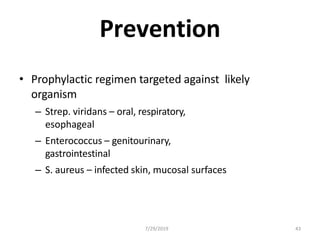
This document provides information on infective endocarditis. It begins by discussing the history and challenges of diagnosing and managing this infection. Key points include that infective endocarditis involves infection of the endothelial surface of the heart. Predisposing factors include dental procedures, infections elsewhere in the body, medical instrumentation, and intravenous drug use. Symptoms can range from acute toxicity and fever to more mild subacute presentations. Echocardiography, blood cultures, and applying the Duke criteria are important for diagnosis. Treatment involves intravenous antibiotics for a prolonged period, sometimes along with surgery for complications. Complications can include embolisms, local or metastatic spread of infection, and immune complex disease. Prevention focuses on prophylactic antibiotics