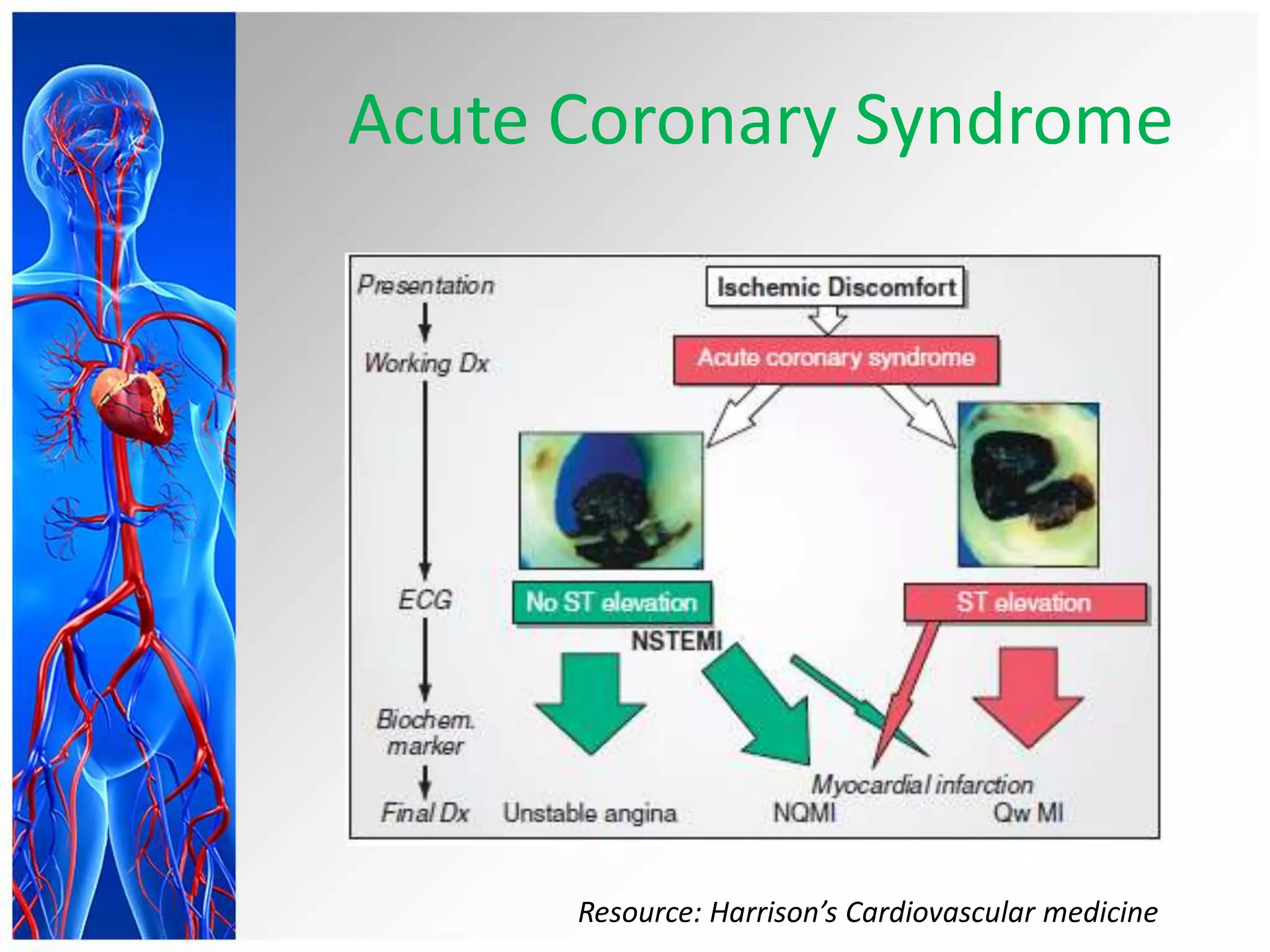
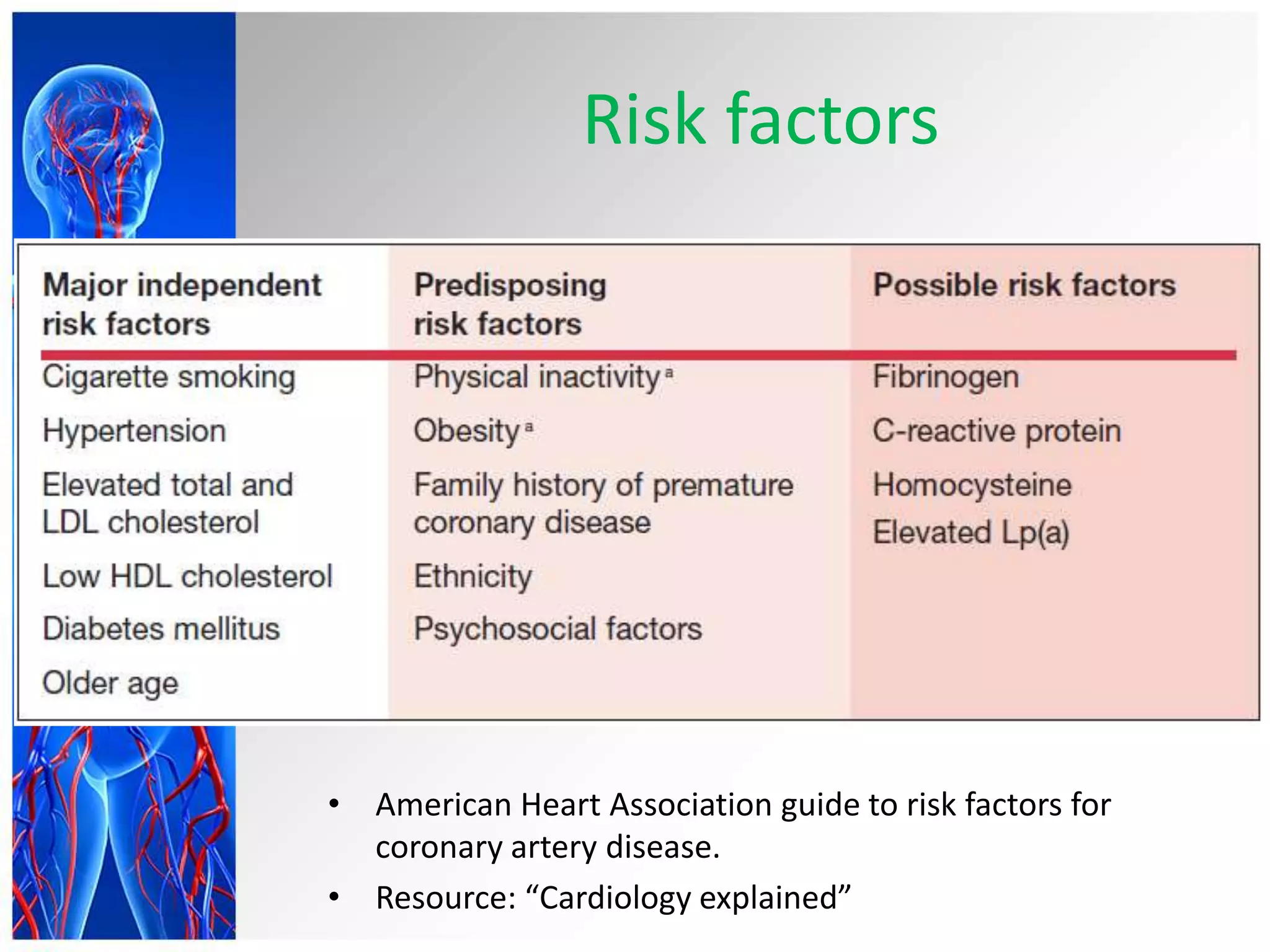
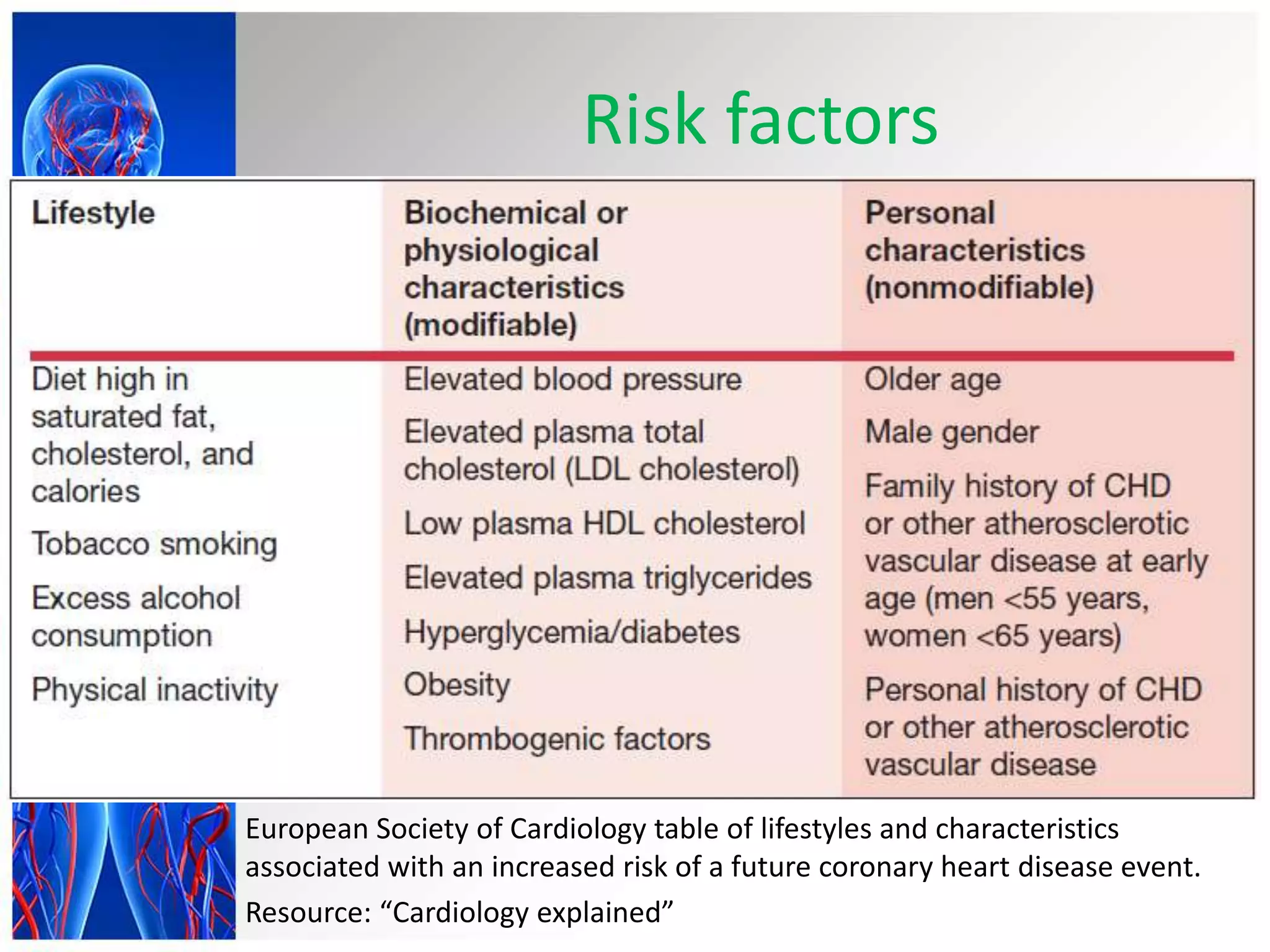
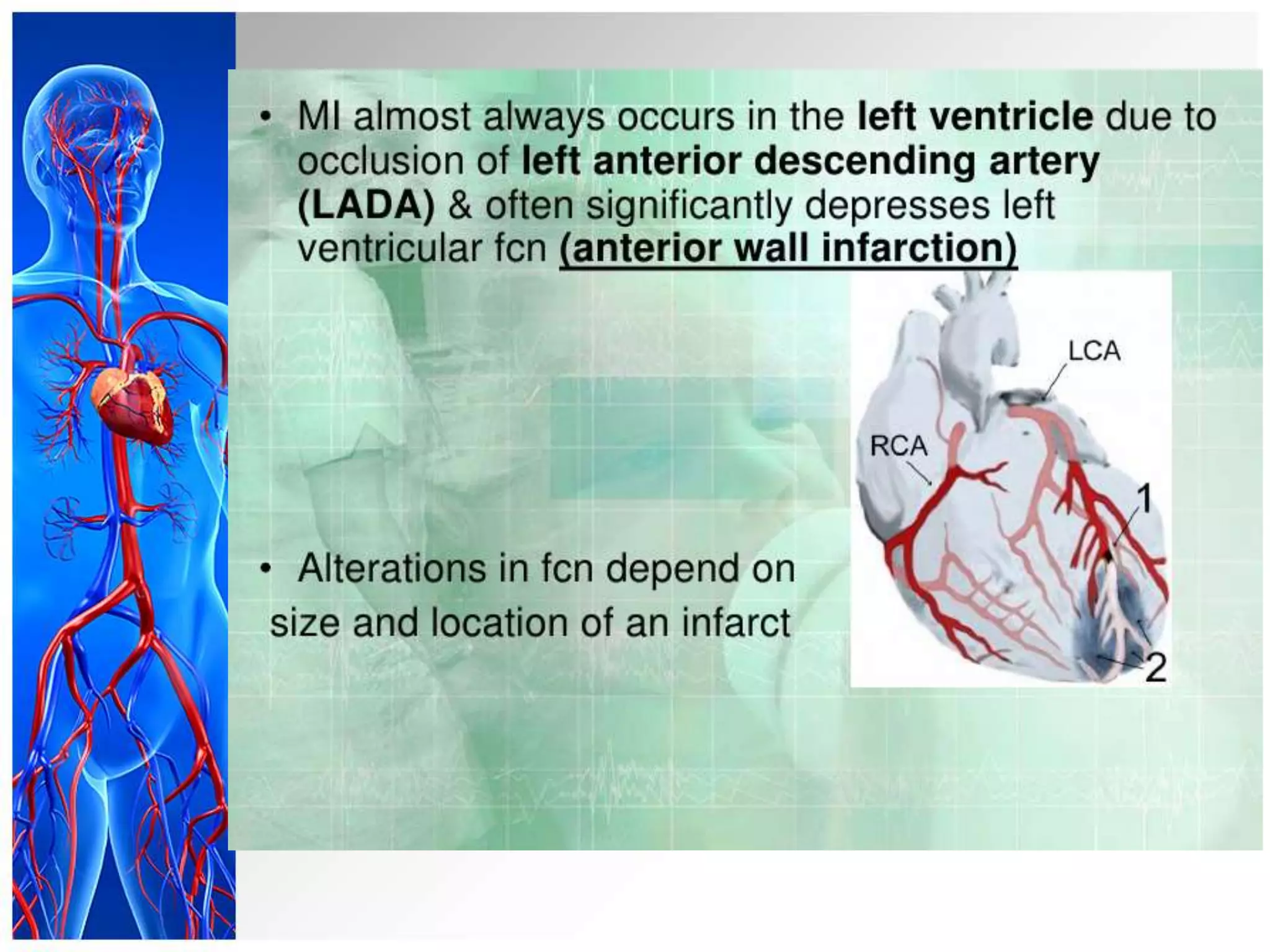
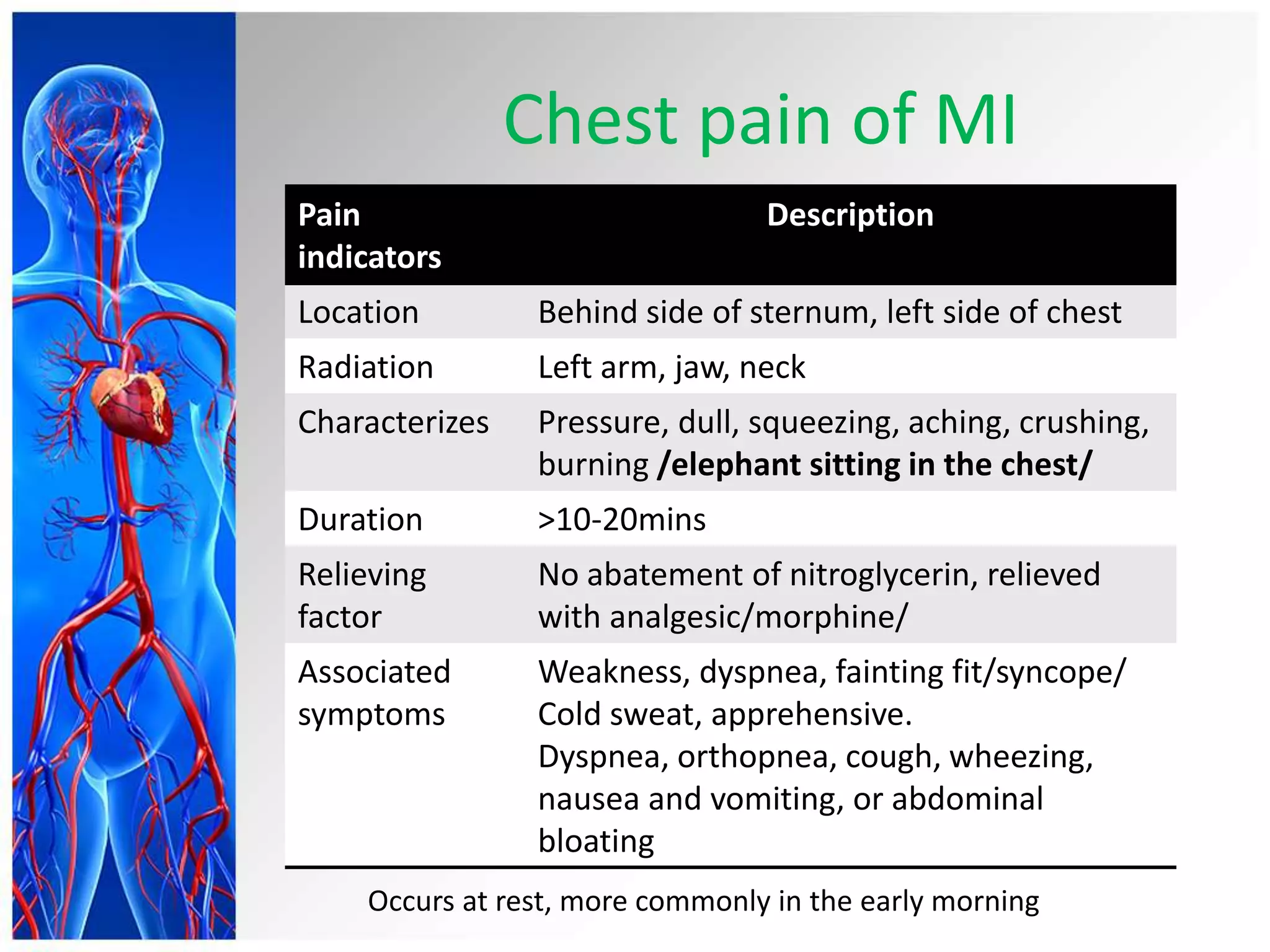
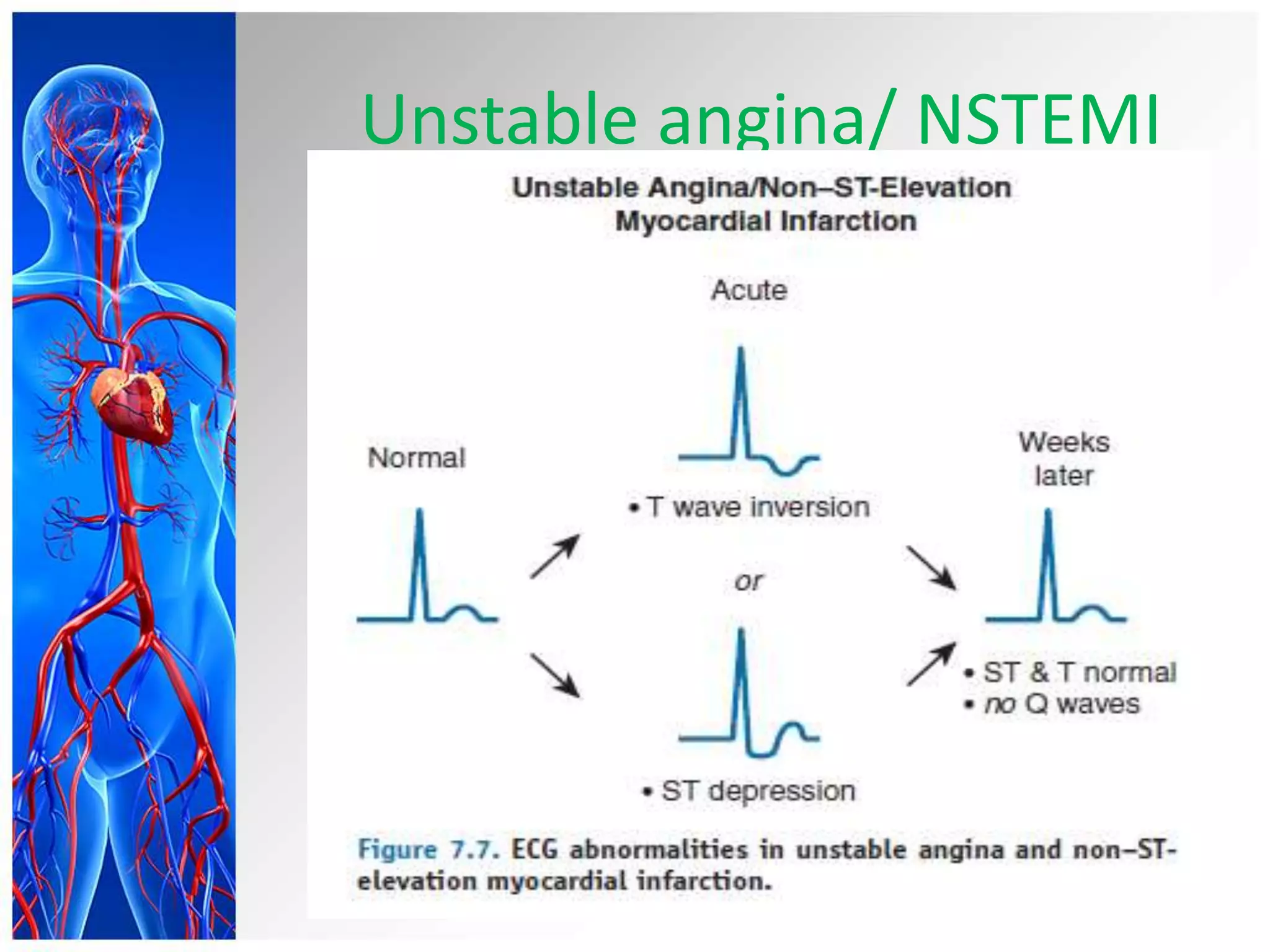
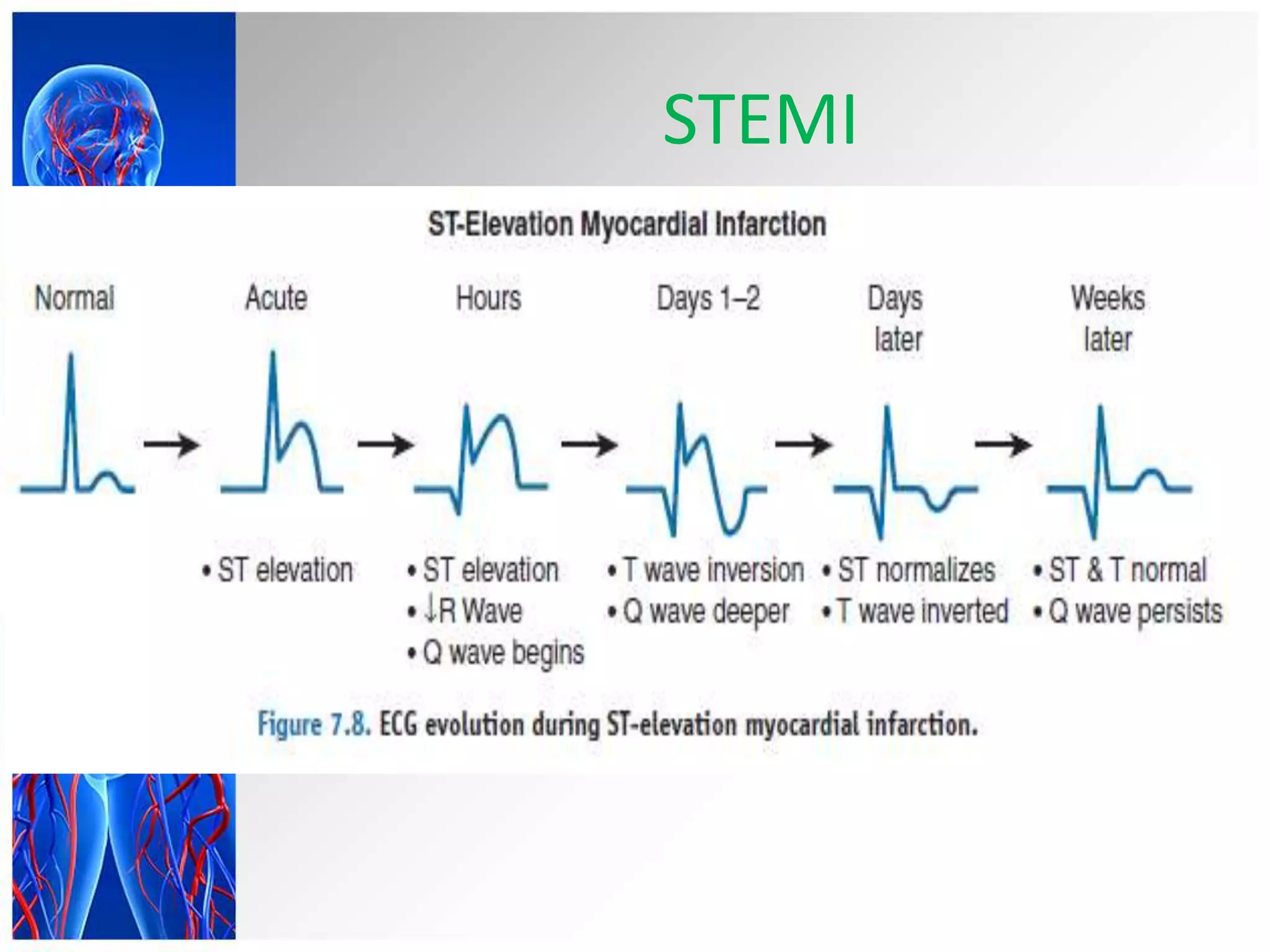
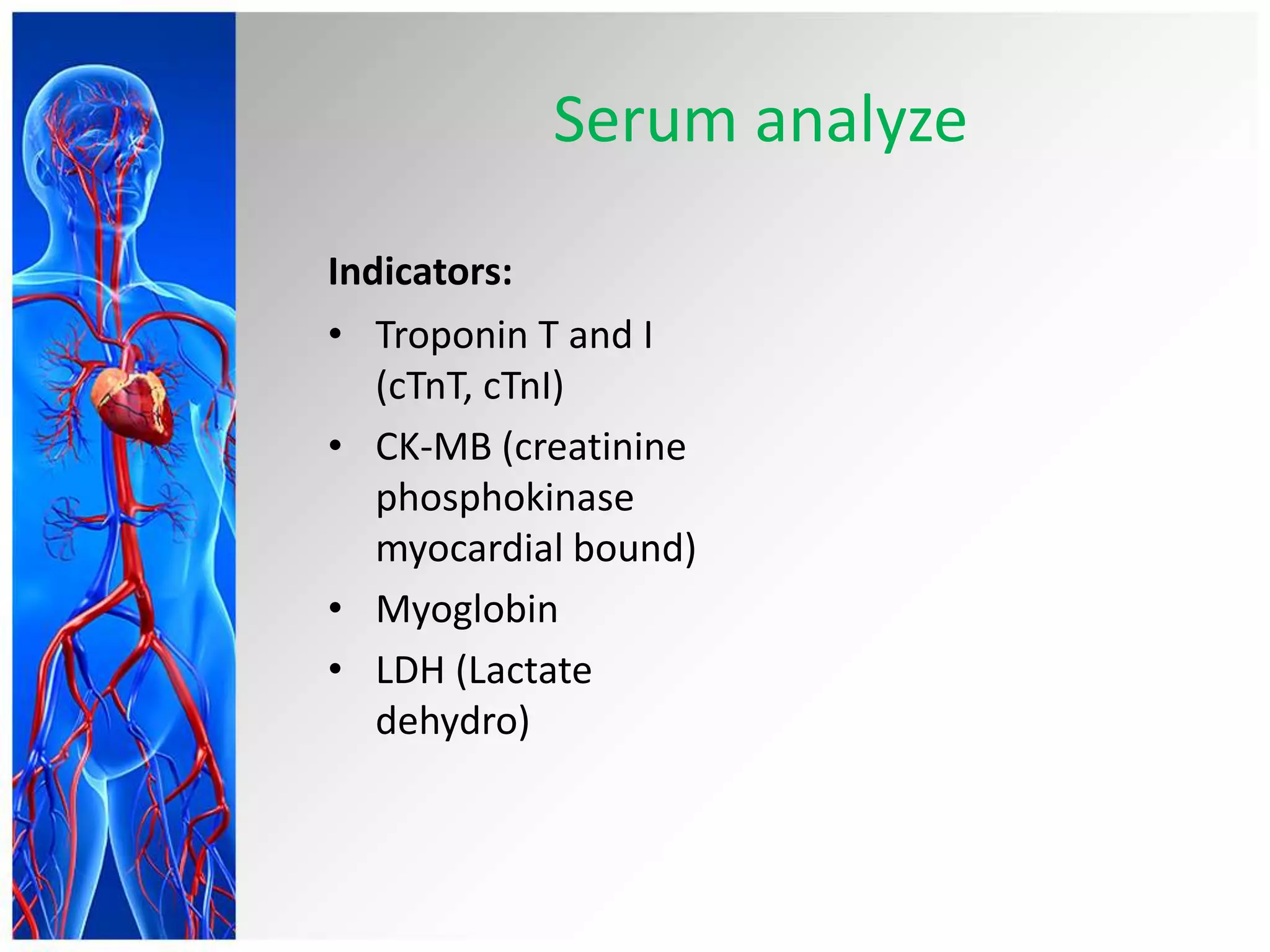
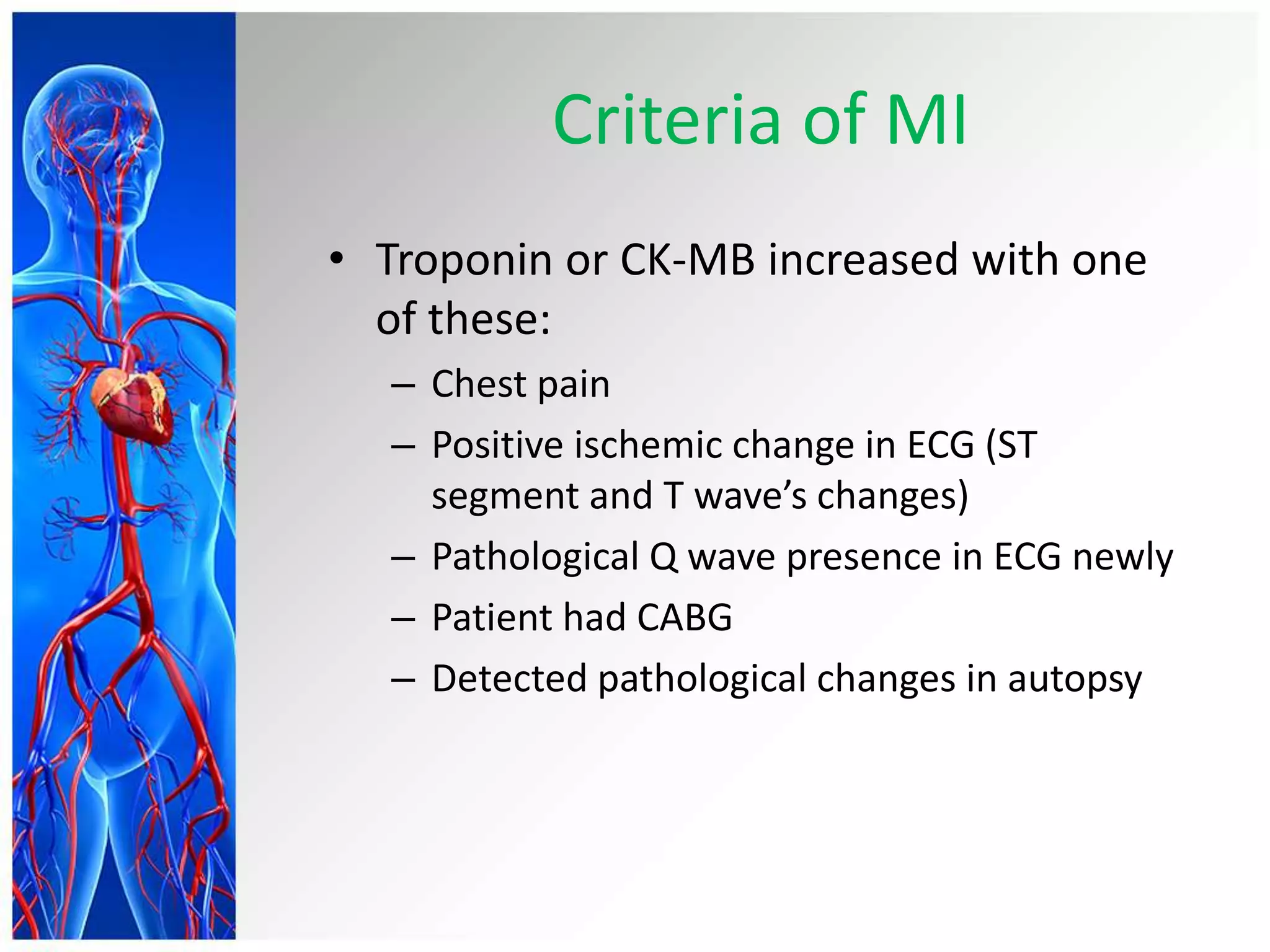
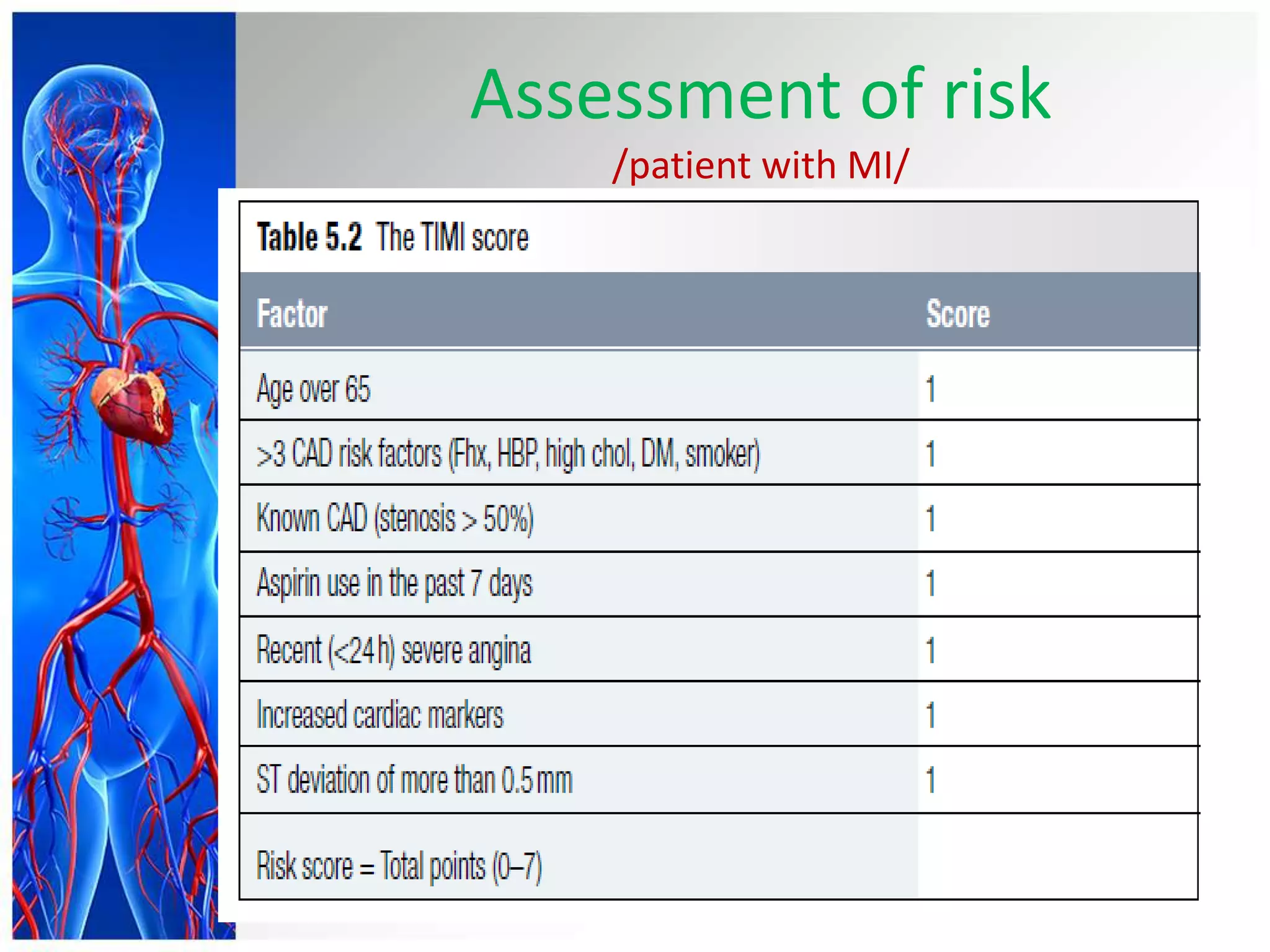
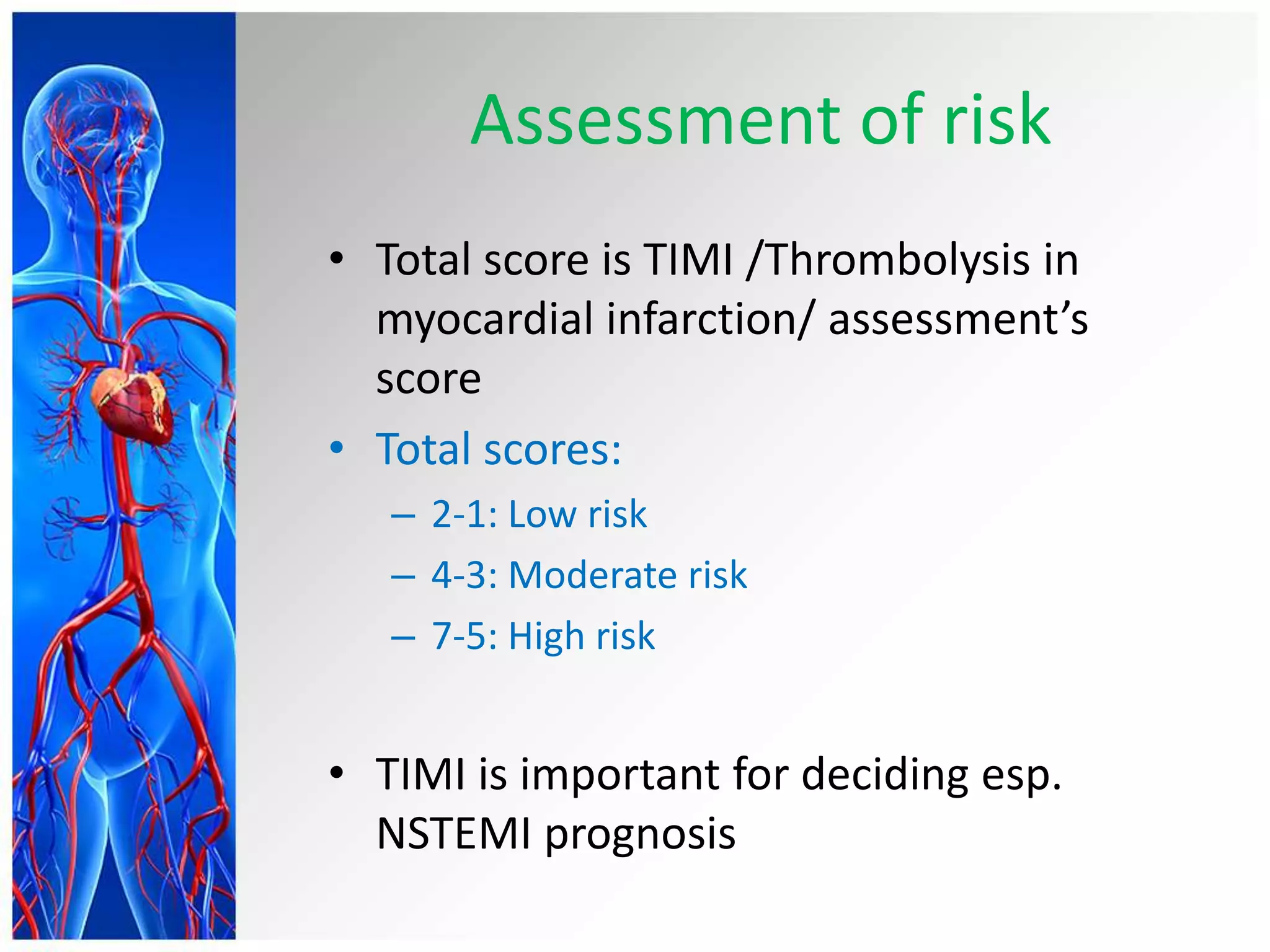
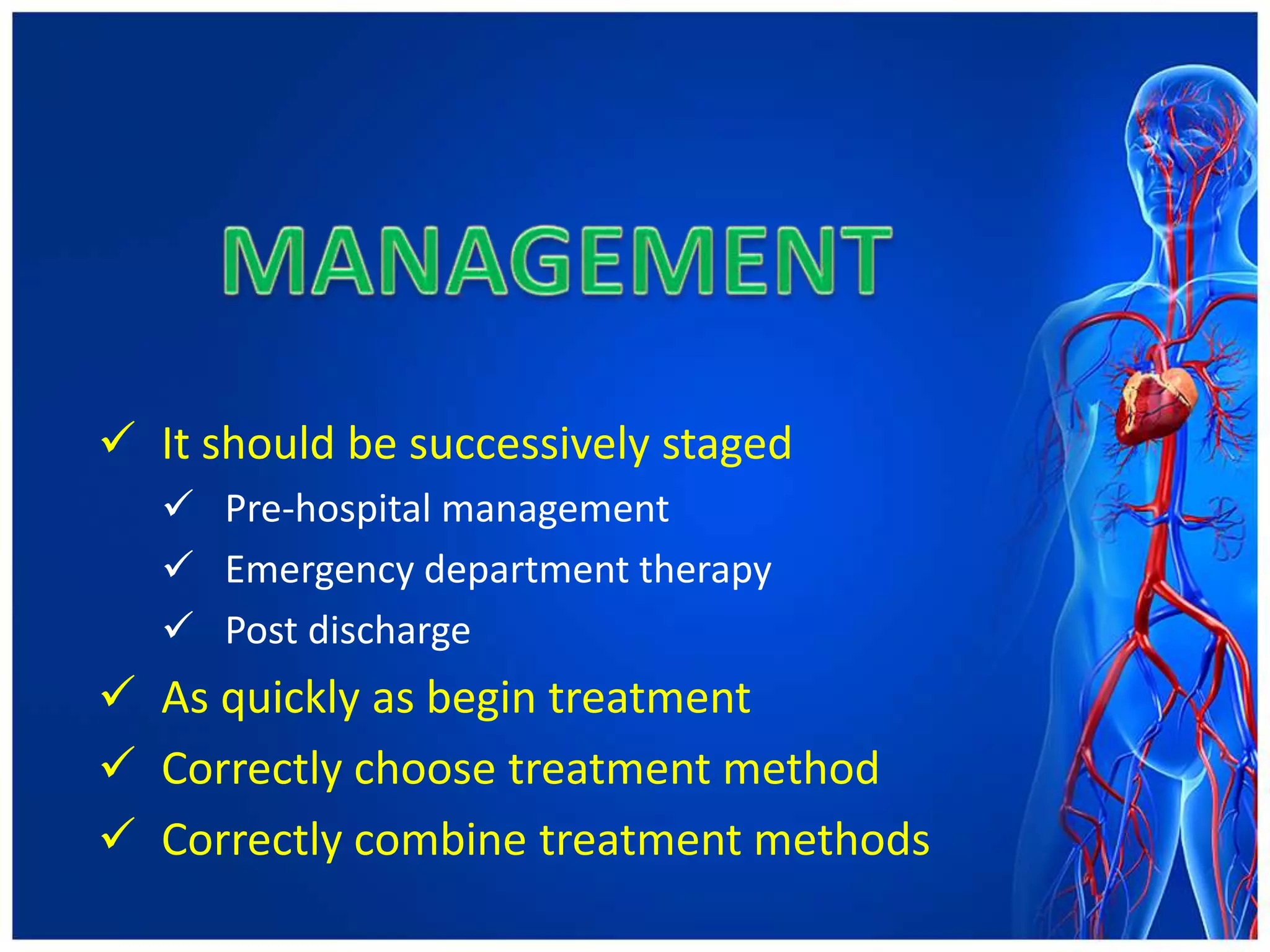
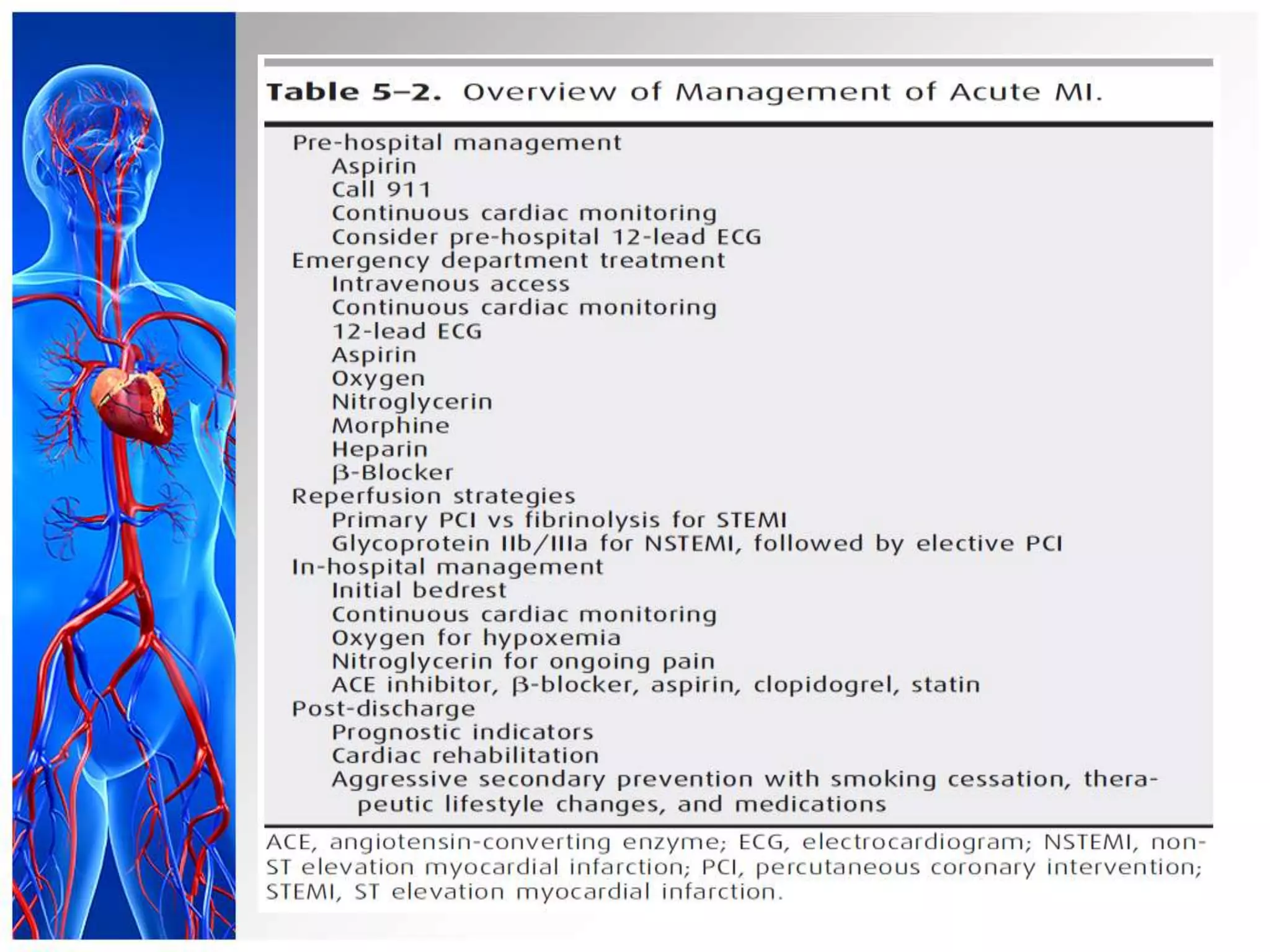
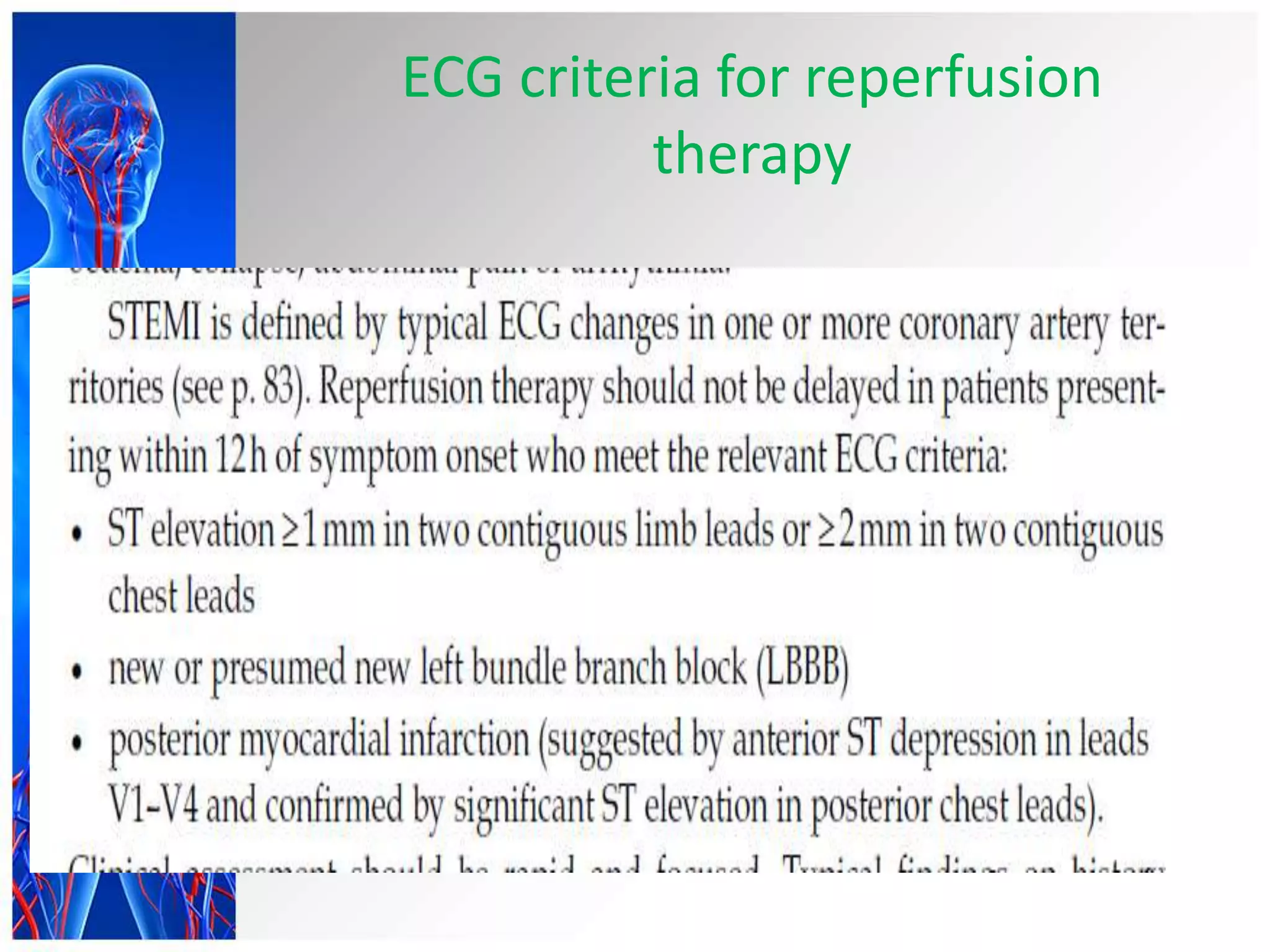
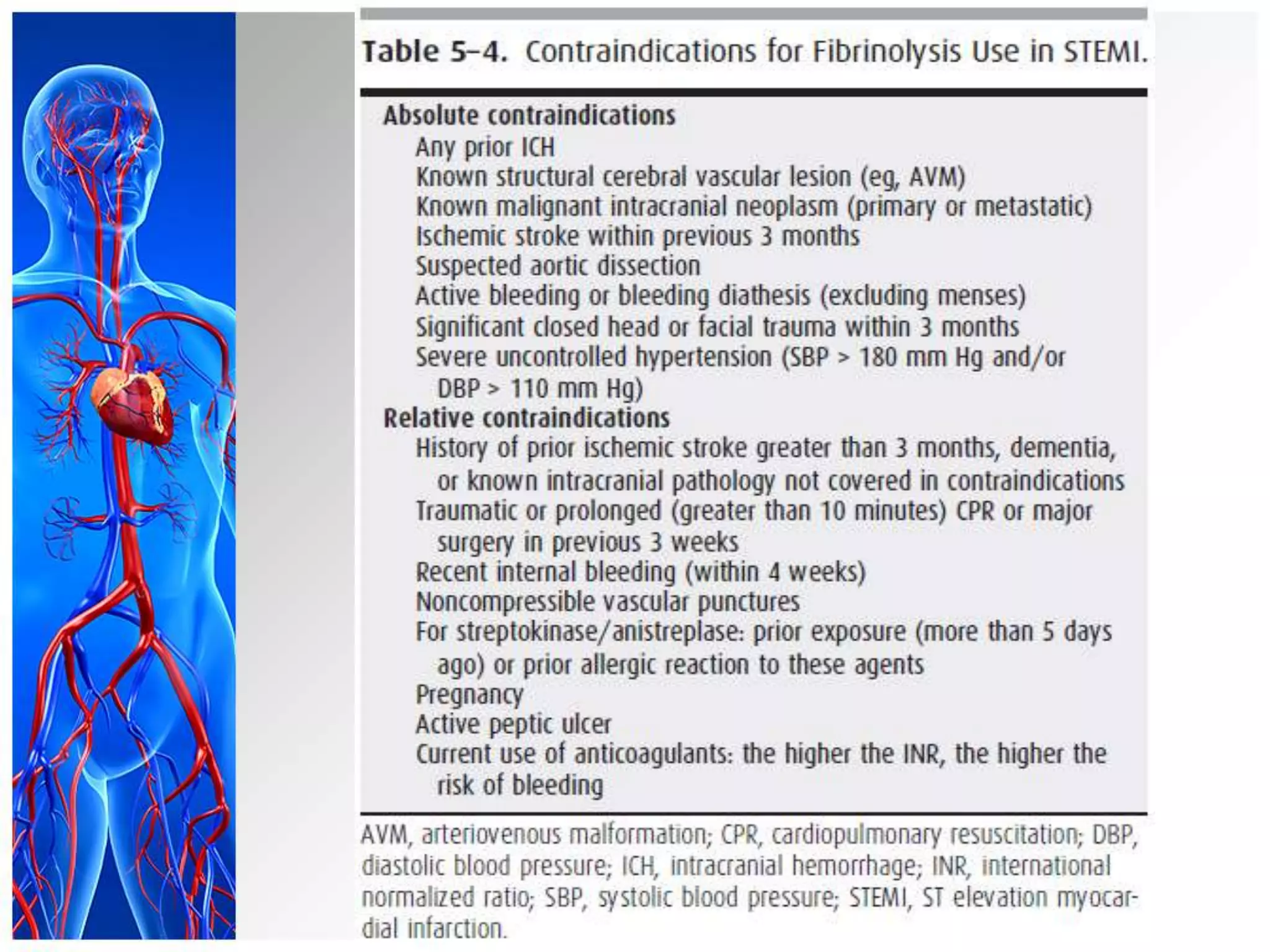
Acute myocardial infarction (MI) results from occlusion of a coronary artery causing death of cardiac myocytes in the supplied region. It is usually caused by atherosclerotic plaque rupture and superimposed thrombus. Risk factors include those associated with coronary artery disease like smoking, hypertension, diabetes, and high cholesterol. MI is classified based on location of damaged tissue as STEMI or NSTEMI/unstable angina and diagnosed through symptoms, electrocardiogram (ECG) changes, and cardiac enzyme levels. Treatment involves pain management, oxygen, nitroglycerin, aspirin, fibrinolytic therapy if indicated, and long-term management of underlying risk factors.