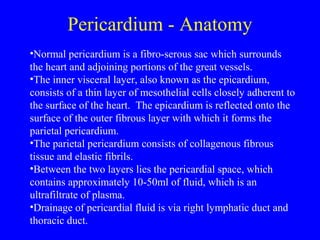
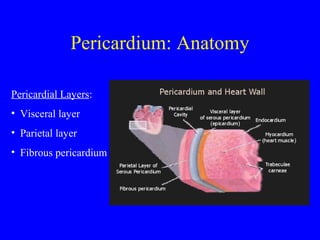
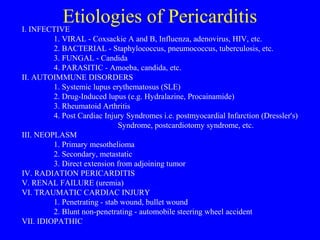
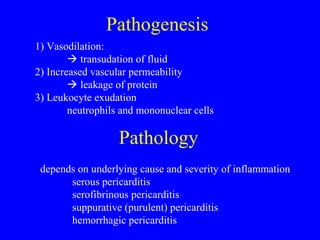
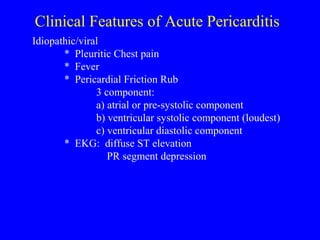
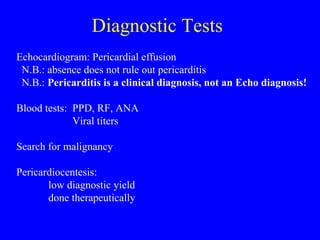
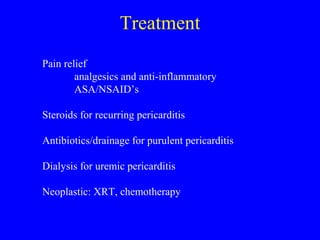
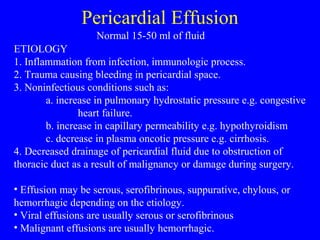
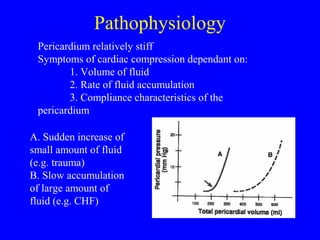
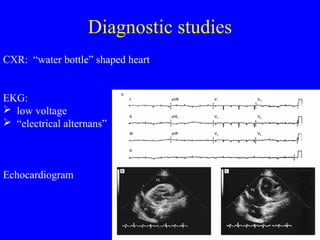
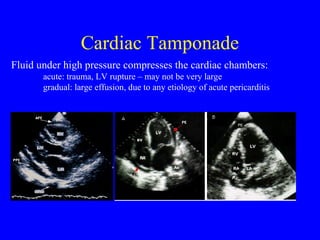
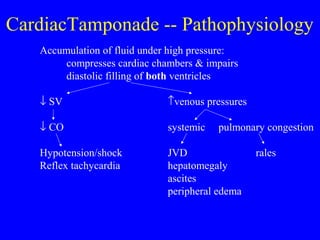
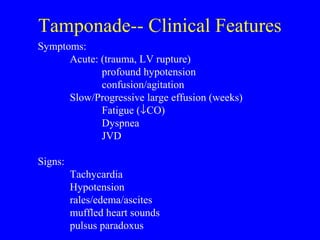
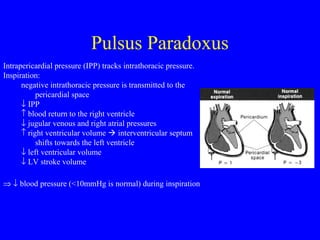
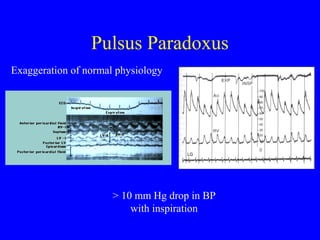
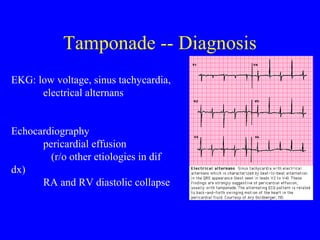
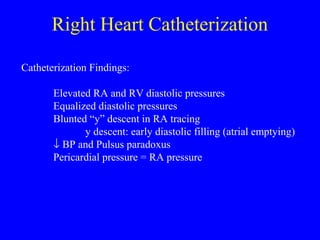
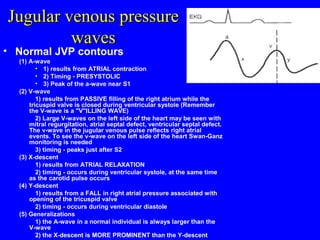
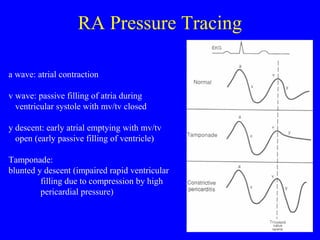
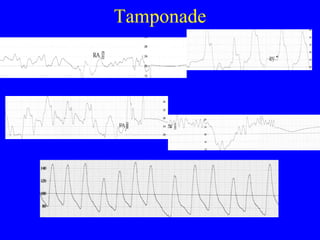
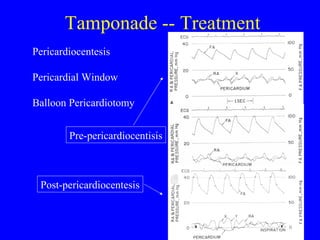
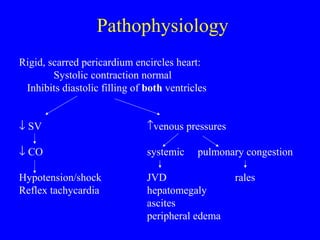
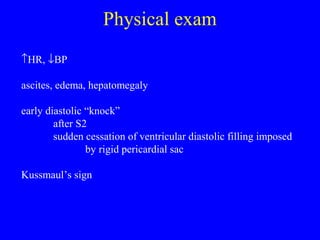
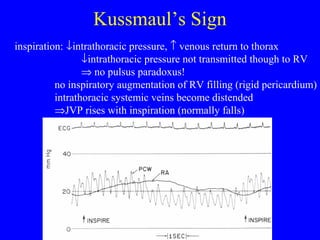
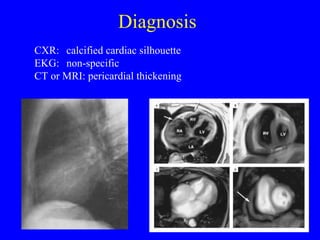
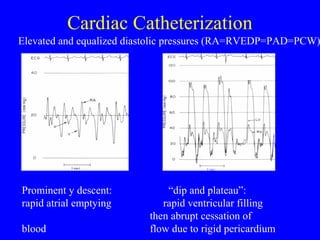
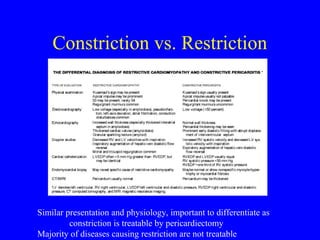
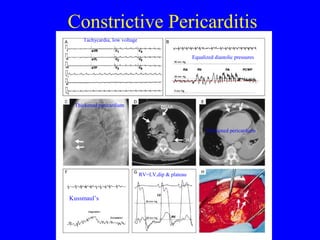
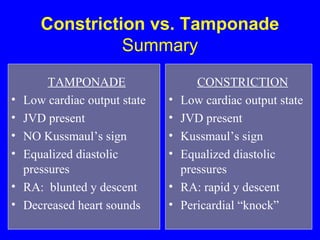
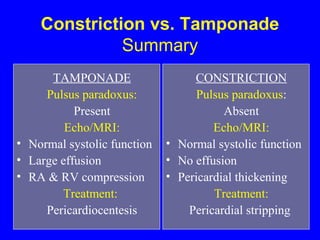
The document discusses the anatomy, functions, pathophysiology, etiologies, clinical features, diagnosis and treatment of pericardial diseases including pericarditis, pericardial effusion, cardiac tamponade, and constrictive pericarditis. Key points include: the pericardium has visceral and parietal layers separated by pericardial fluid; pericarditis can be caused by infection, autoimmune disorders, neoplasms or trauma; tamponade occurs when fluid rapidly accumulates under pressure, compressing the heart; constrictive pericarditis involves fibrosis and scarring that restricts diastolic filling.