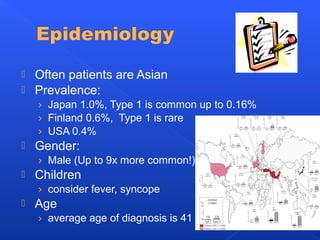
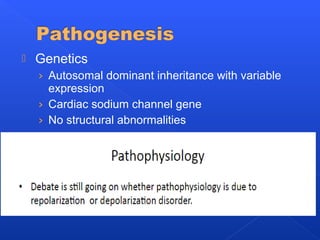
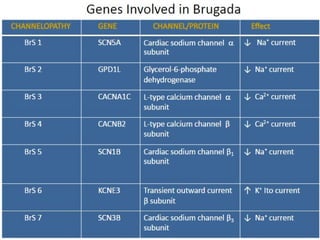
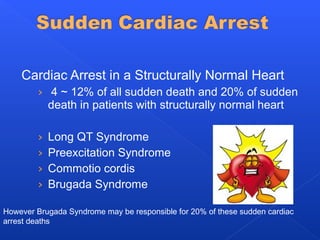
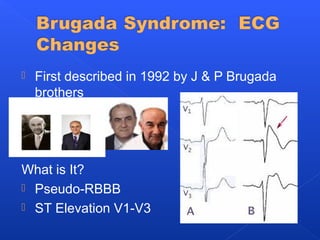
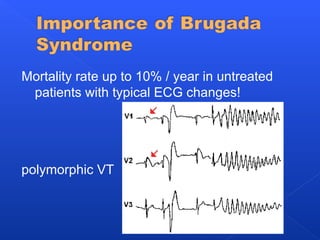
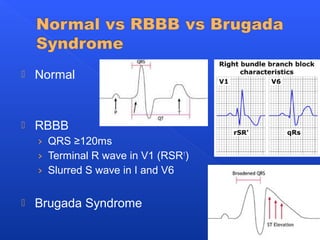
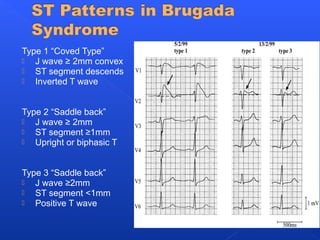
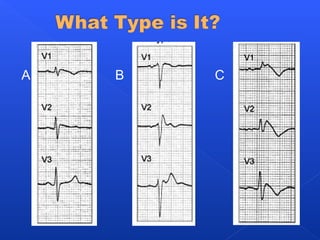
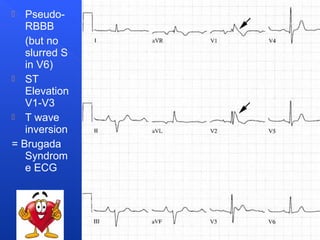
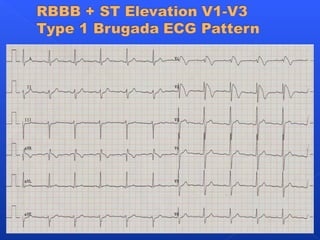
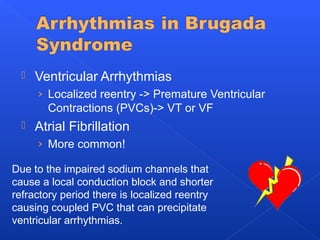
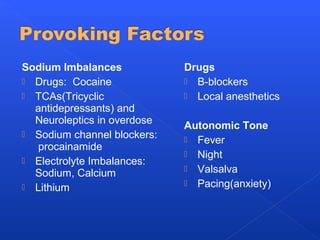
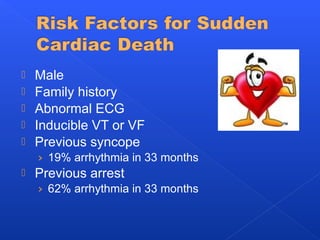
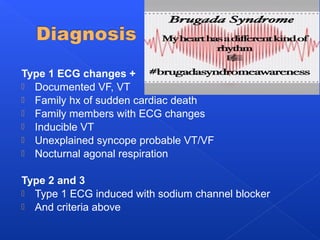
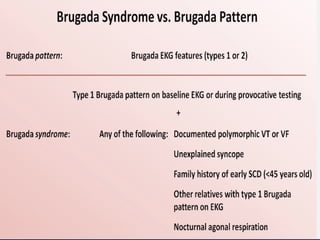
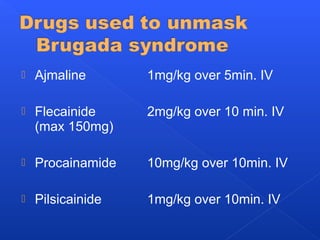
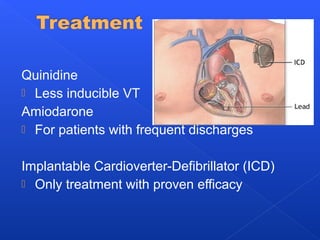
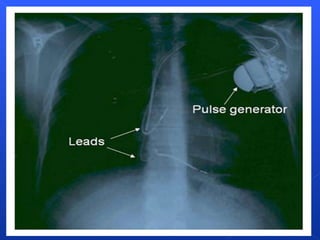
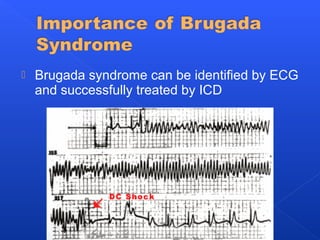
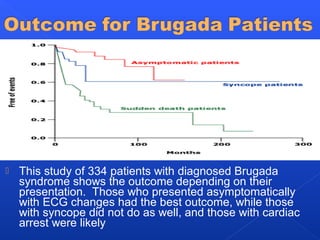
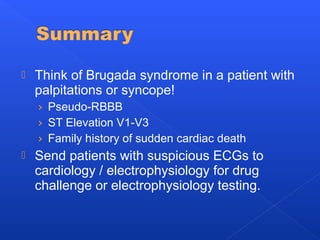
This document discusses Brugada syndrome, a condition characterized by abnormal ECG findings and increased risk of sudden cardiac death. It presents information on the epidemiology, pathogenesis, diagnosis, and treatment of Brugada syndrome. Key points include that it is more common in males and Asians, and symptoms can include palpitations or syncope. Diagnosis involves specific ECG patterns and drug challenge may be used. Treatment focuses on managing arrhythmias using medications like quinidine or implantable cardioverter-defibrillators, with the latter being the only proven effective treatment.