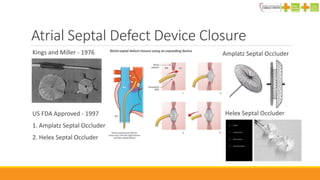
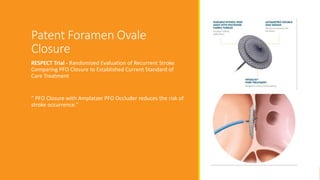
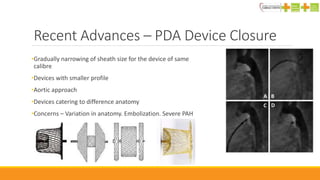
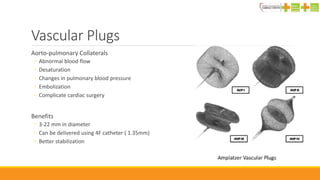
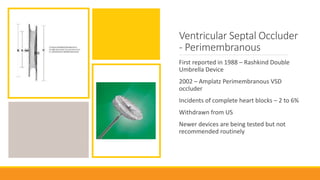
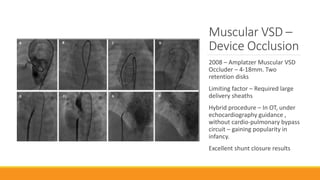
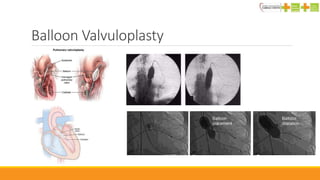
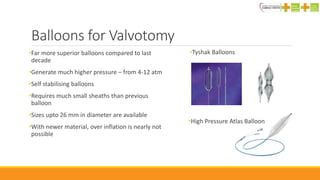
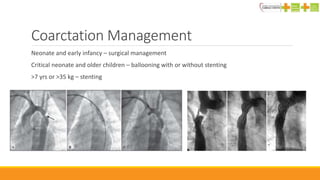
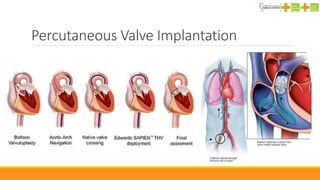
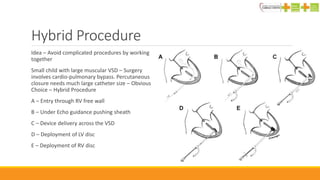
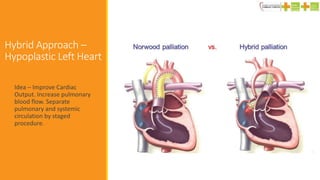
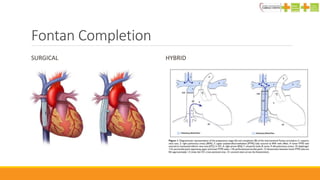
Recent advances in interventional pediatric cardiology include improving existing techniques such as atrial septal defect closure and balloon valvuloplasty, developing new methods like percutaneous pulmonary valve replacement, and exploring hybrid procedures combining surgery and catheterization. New devices now allow closure of defects that were previously not suitable for catheter procedures. Stenting has expanded the options for treating lesions like coarctation of the aorta. Overall, interventional techniques are helping manage more complex congenital heart disease with less invasive approaches.