This document defines and describes infective endocarditis. Key points include:
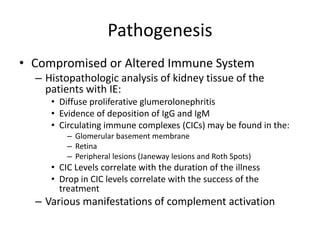
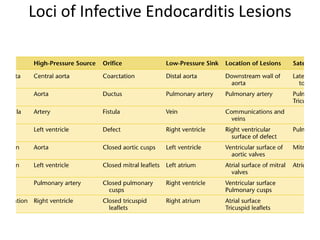
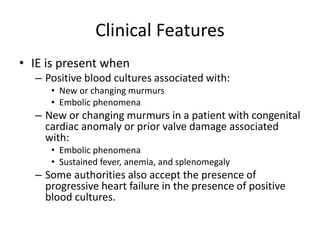
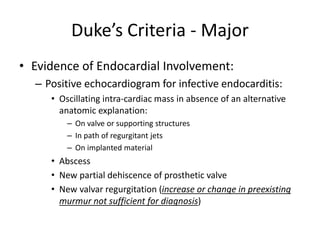
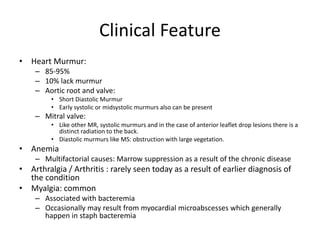
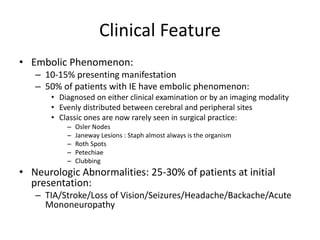
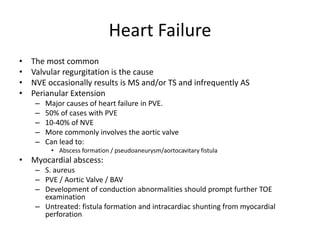
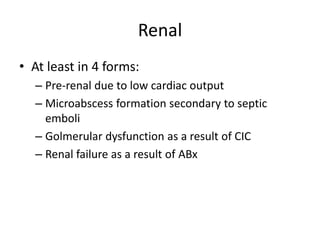
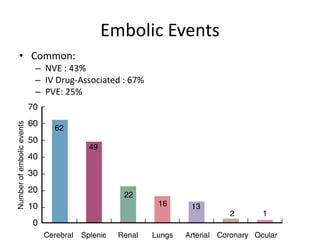
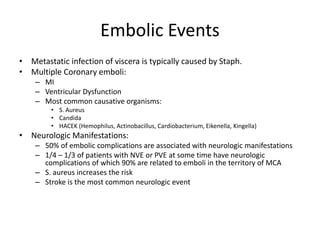
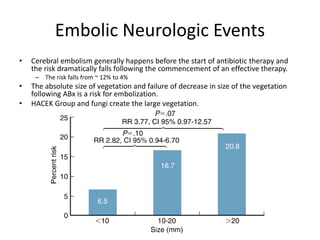
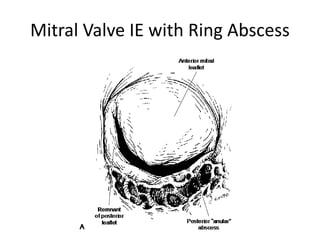
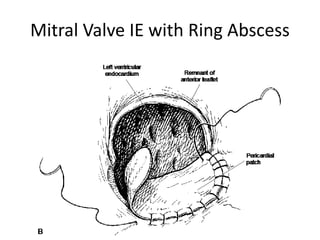
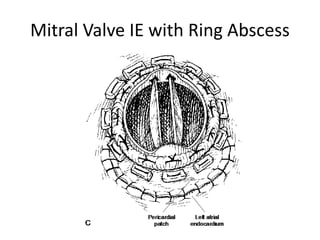
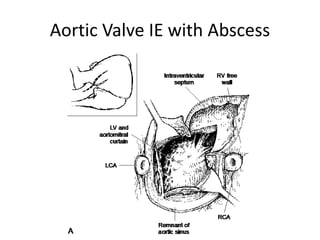
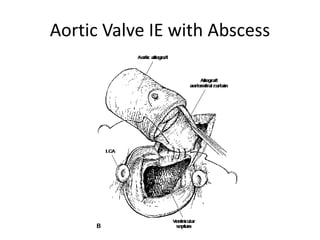
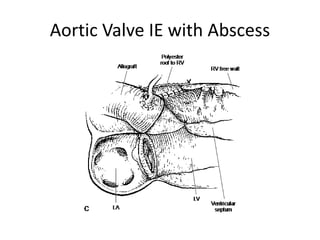
- Infective endocarditis involves infection of the heart valves or structures, most commonly the valves. This can lead to valvular dysfunction, sepsis, or embolism.
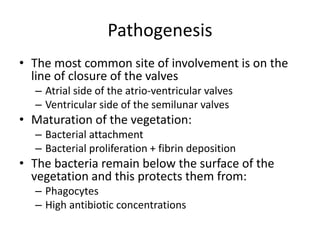
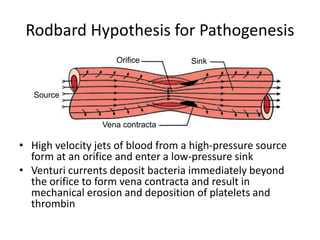
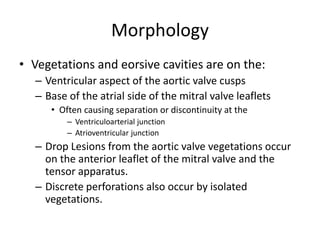
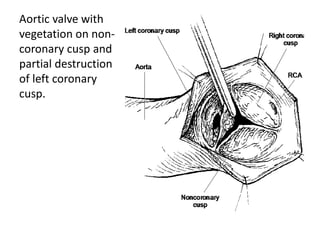
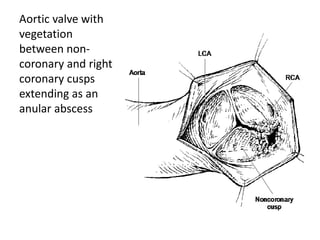
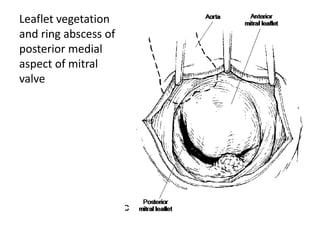
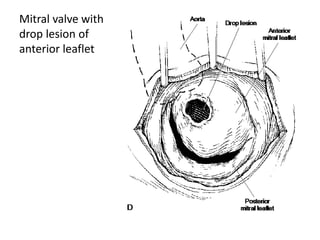
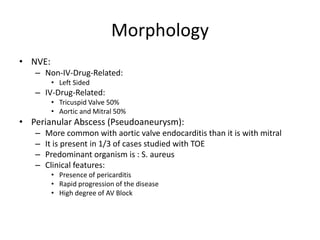
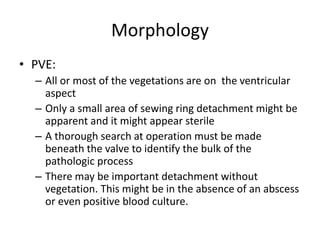
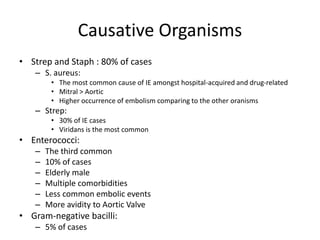
- The infection involves bacterial, viral, or fungal invasion of the endocardium and formation of vegetations on the valves or endocardium.
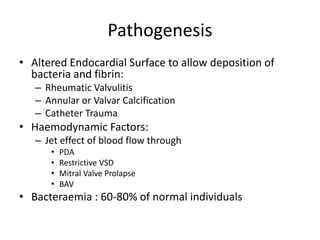
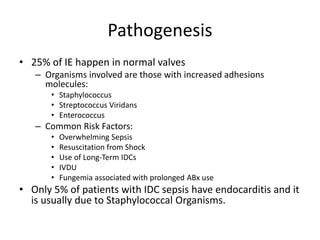
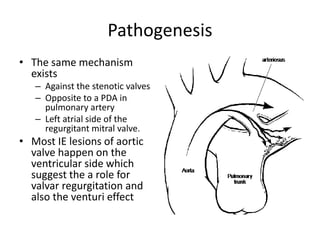
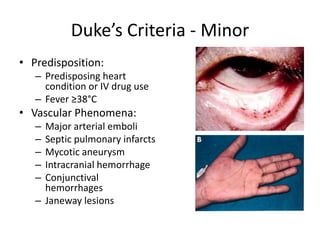
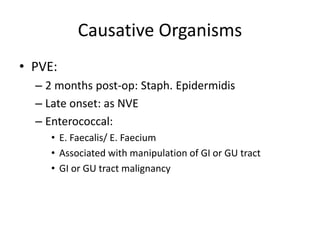
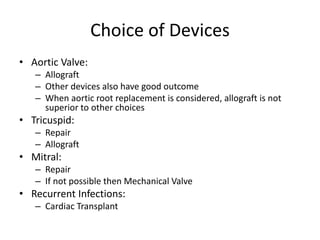
- Risk factors include underlying heart conditions, IV drug use, dental procedures, and indwelling catheters. The aortic and mitral valves are most commonly involved.
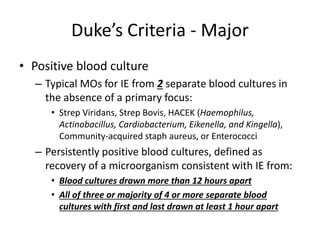
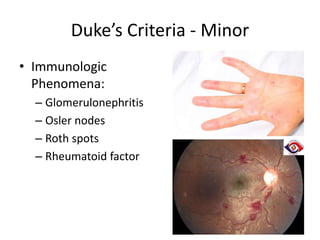
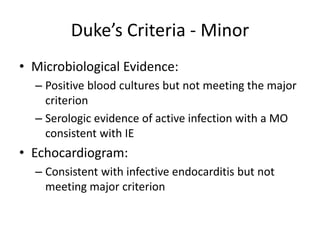
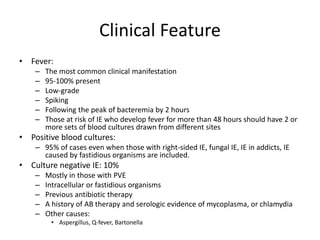
- Symptoms may include fever, heart murmur, embolic phenomena, and heart failure. Diagnosis