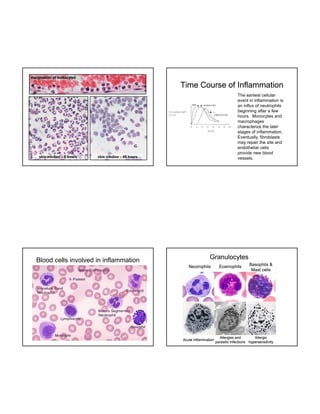
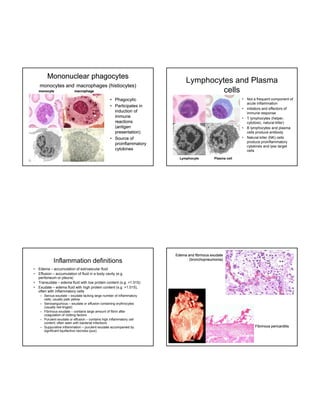
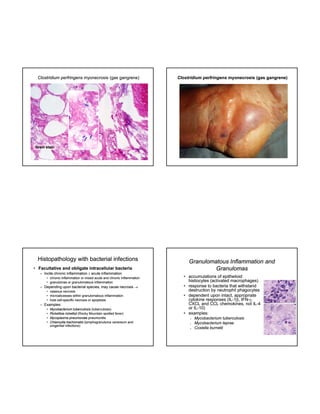
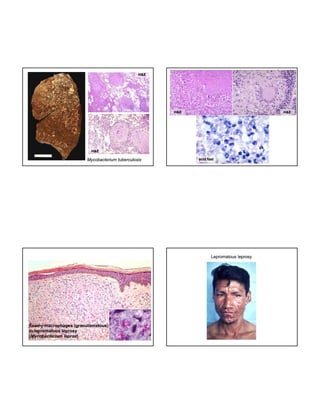
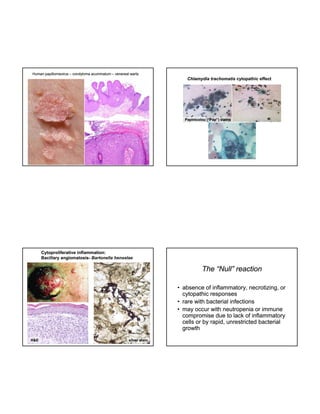
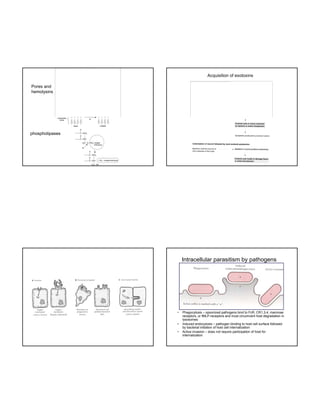
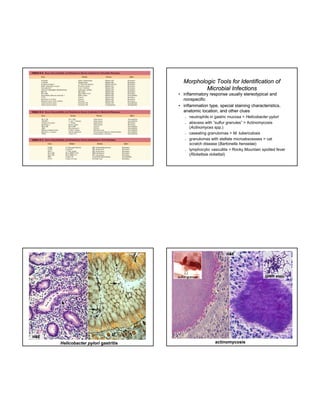
The document discusses host responses to microbial pathogens, detailing both innate and adaptive immunity. It covers key mechanisms of inflammation, types of inflammatory responses, and the various bacterial factors that influence disease processes, including exudative and necrotizing inflammation. Additionally, it outlines bacteria's strategies to evade host defenses and the histopathological features associated with different infections.