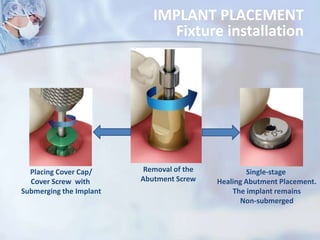
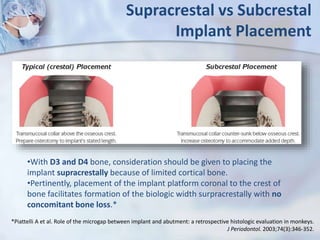
This document discusses key principles of implant surgery, including atraumatic bone preparation with irrigation to minimize heat, achieving primary stability through bicortical stabilization, and allowing undisturbed osseointegration. It also covers preoperative mouthwash and skin disinfection, antibiotic prophylaxis, and using nerve block anesthesia or infiltration anesthesia. Precise drilling techniques aim to expose bone for osteotomy while minimizing vascular disruption. Implant placement involves creating the osteotomy with intermittent drilling, using correct torque values, and placing the implant fixture by hand or with a controlled drill.