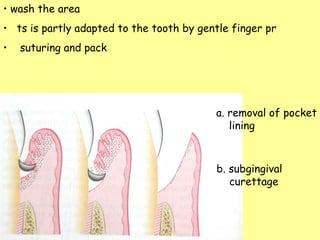
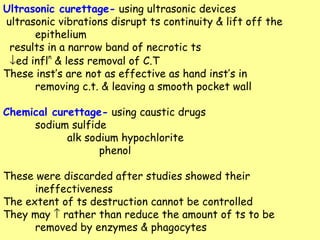
The document discusses gingival curettage, which involves scraping the lining of periodontal pockets to remove diseased soft tissue. It aims to reduce pocket depth and promote new connective tissue attachment. Gingival curettage specifically refers to removing tissue lateral to the pocket wall, while subgingival curettage is performed below the epithelial attachment to sever the connection to bone. The document outlines the procedure, healing process, indications, contraindications and potential complications of gingival curettage.