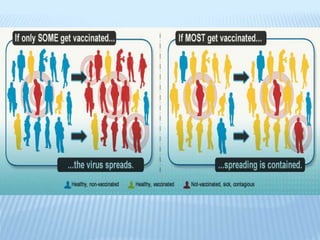
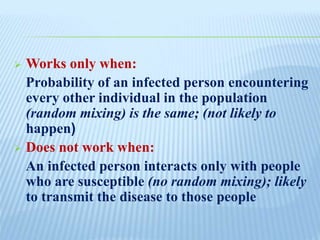
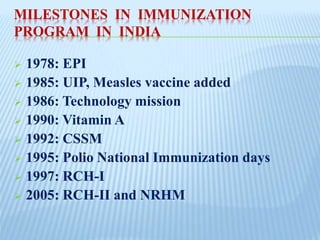
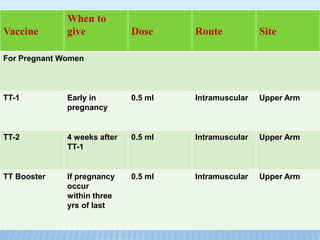
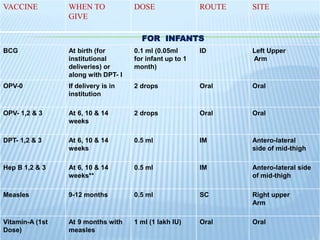
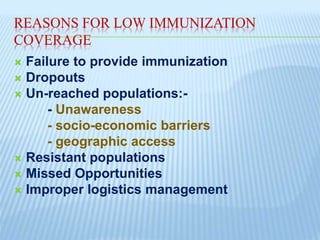
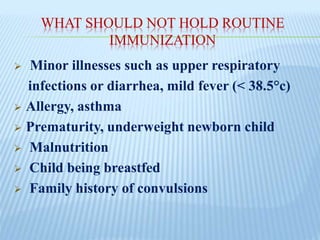
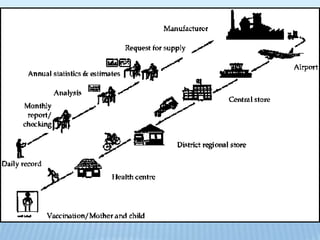
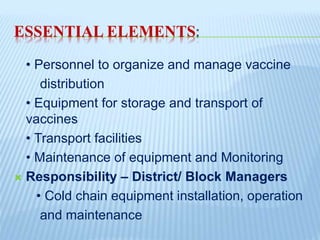
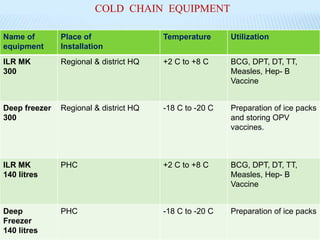
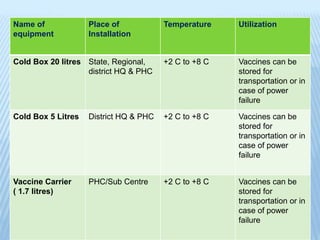
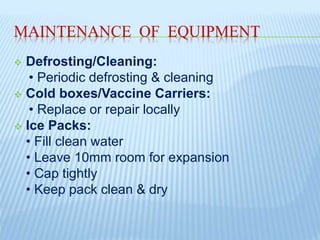
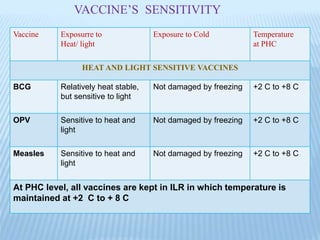
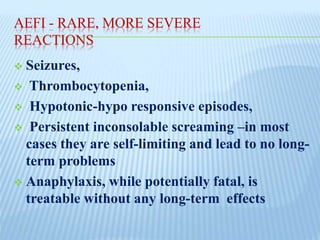
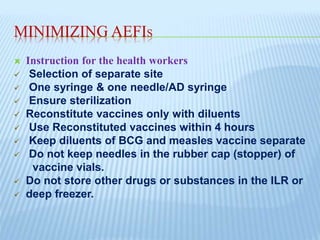
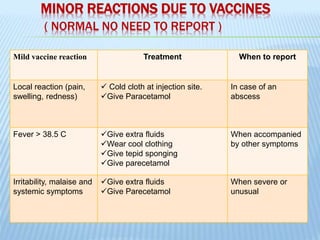
This document discusses immunization and vaccines. It begins by outlining the importance of immunization for child survival and lowering morbidity and mortality rates. It then defines key terms like immunization, immunity, vaccine, and vaccination. It provides details on full and partial immunization schedules for children and mothers. It discusses herd immunity and milestones in India's immunization program. It also covers barriers to immunization, reasons for low coverage, guidelines for routine immunization, and the cold chain system. Finally, it discusses adverse events following immunization and how to minimize their occurrence.