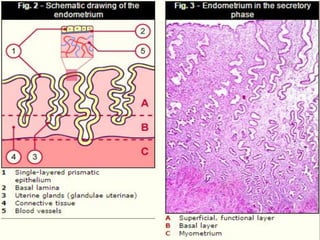
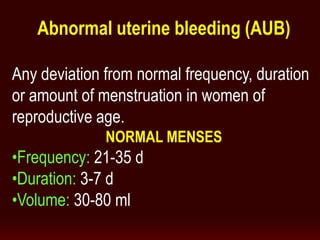
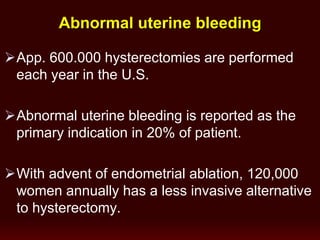
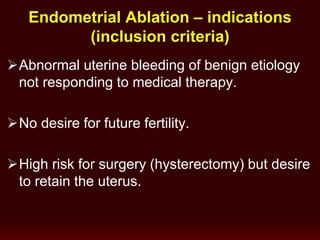
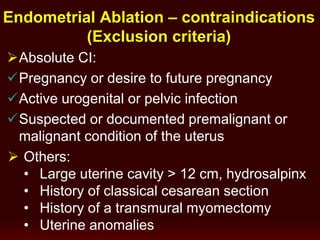
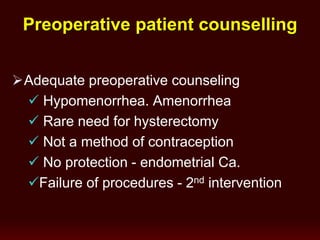
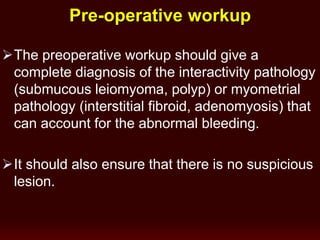
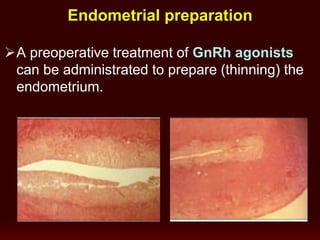
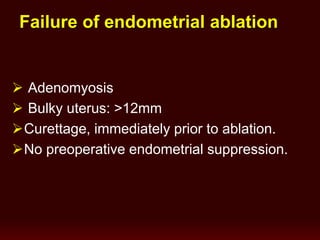
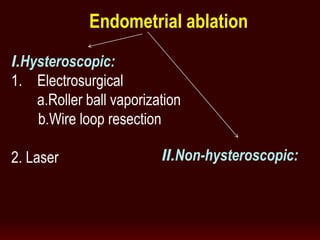
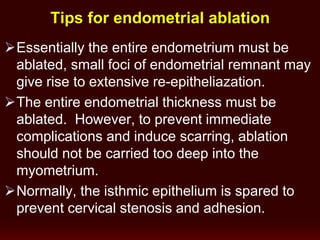
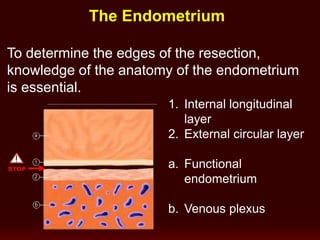
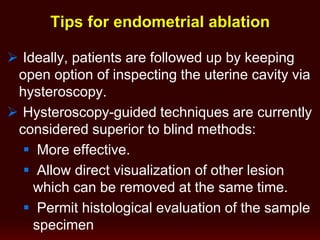
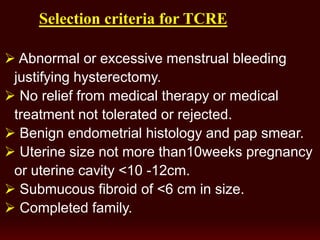
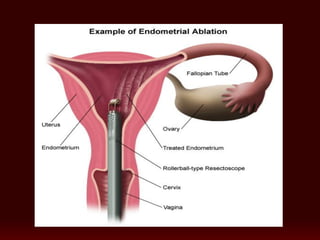
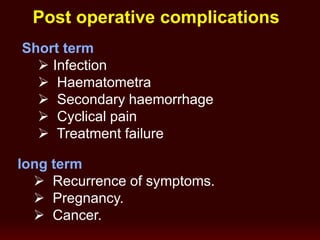
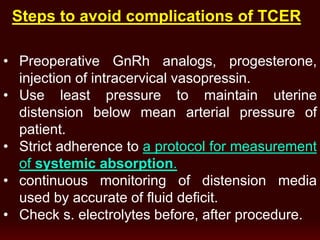
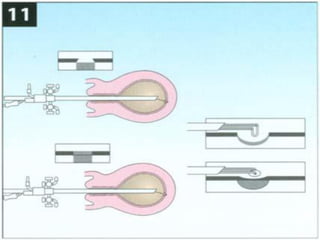
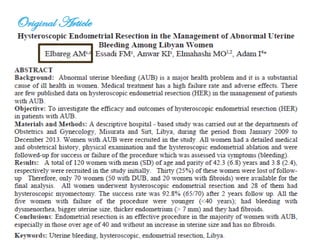
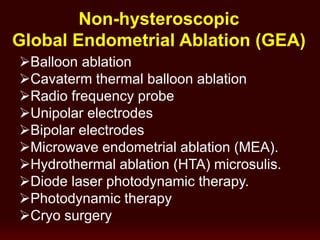
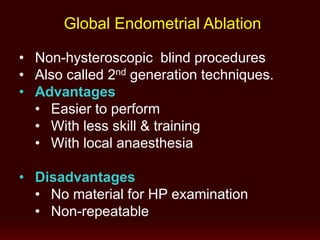
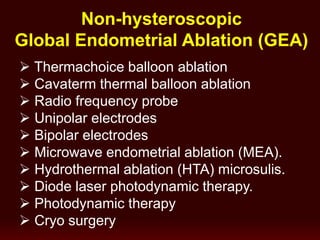
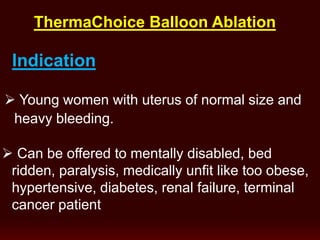
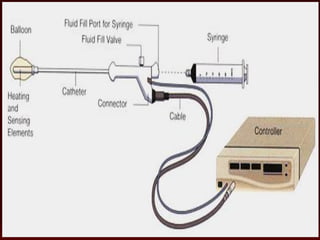
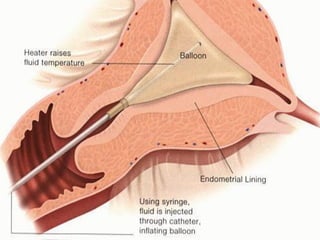
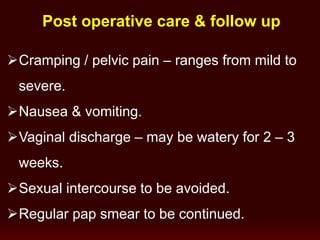
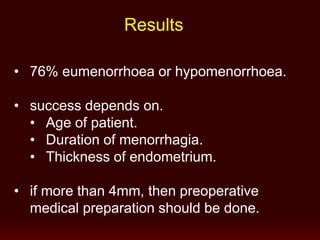
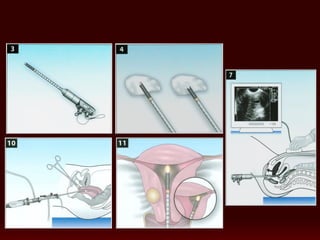
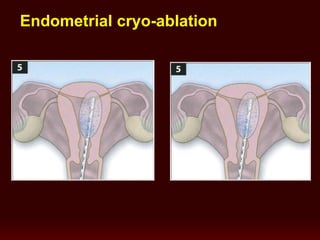
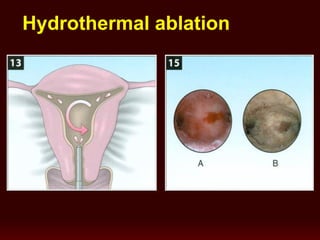
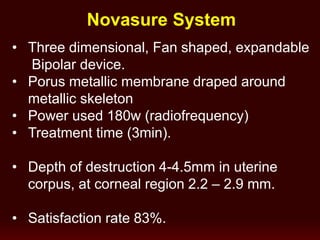
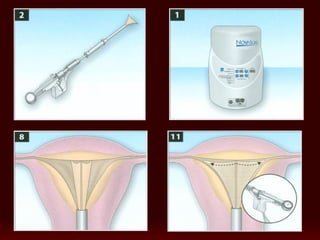
This document discusses endometrial ablation, which is a treatment for abnormal uterine bleeding where the endometrium is destroyed. It notes that endometrial ablation has advantages over hysterectomy as it is less invasive, allows the uterus to be preserved, and has a shorter recovery time. The document provides details on the various techniques for endometrial ablation and notes it is most effective when performed hysteroscopically to allow direct visualization. Preparation of the endometrium and cervix is recommended to improve outcomes.