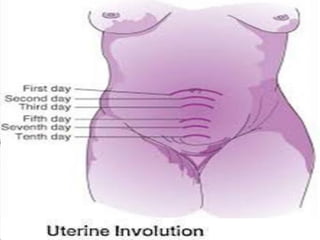
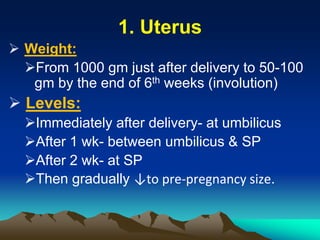
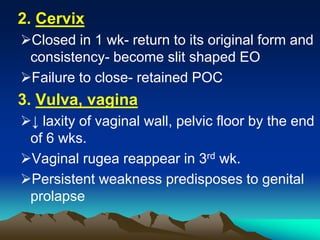
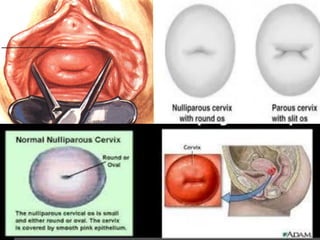
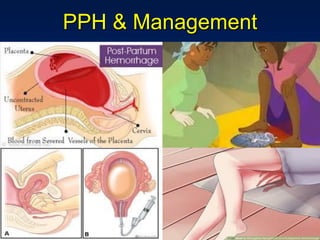
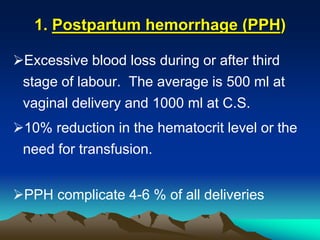
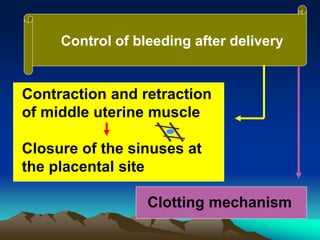
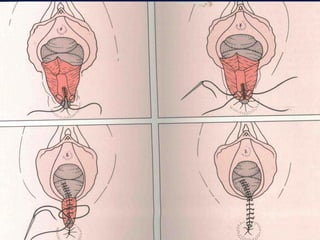
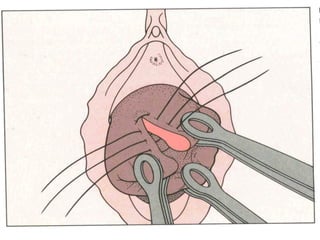
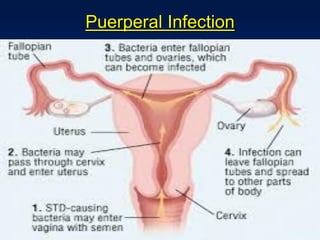
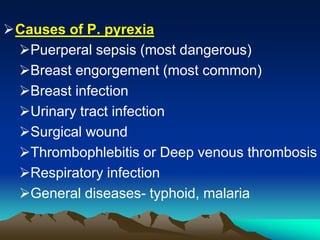
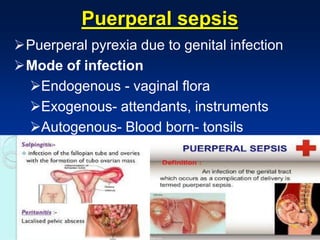
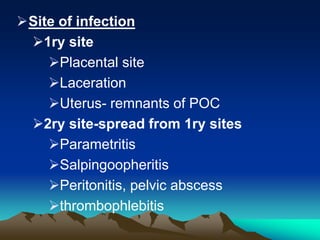
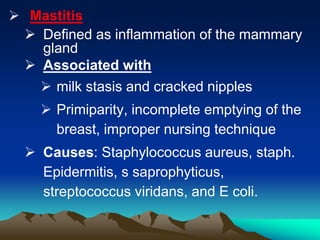
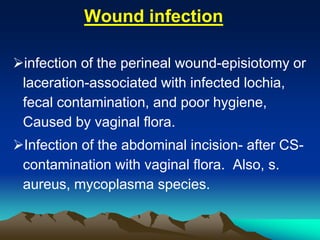
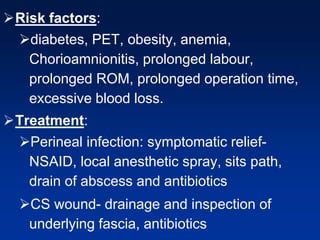
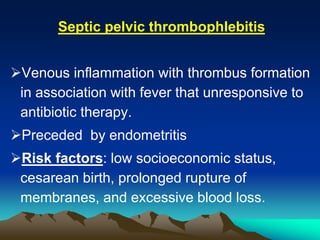
This document discusses normal puerperium and some abnormalities that can occur. The postpartum period is divided into three stages: immediate (first 24 hours), early (first week), and remote (up to 6 weeks). Physiological changes that occur include uterine involution and return of other systems like temperature and blood pressure to pre-pregnancy levels. Potential abnormalities covered include postpartum hemorrhage, puerperal pyrexia (infection), painful perineum, and psychological disorders. Causes, signs, and management are described for these complications.