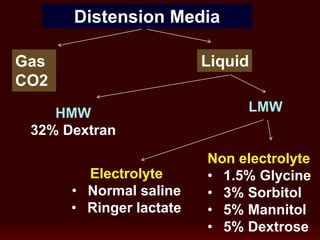
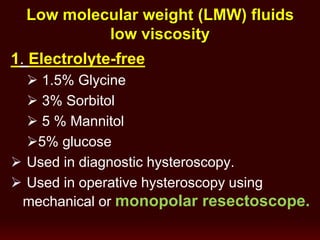
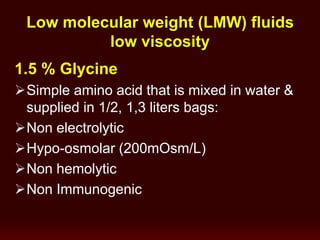
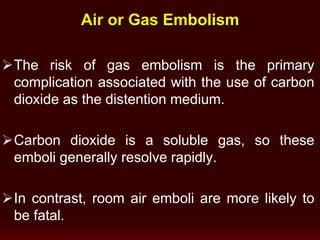
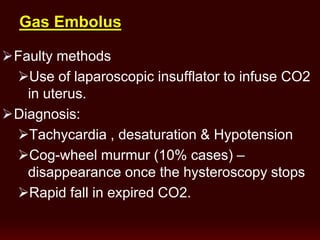
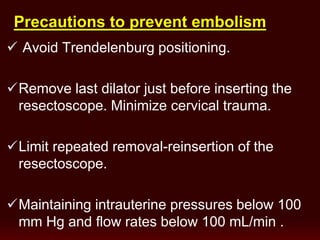
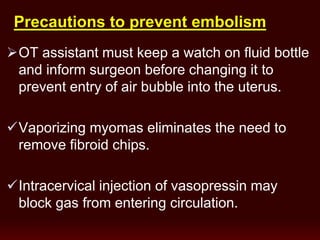
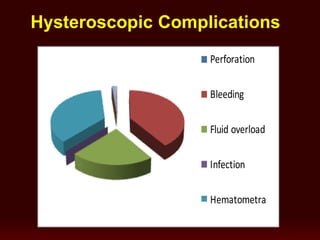
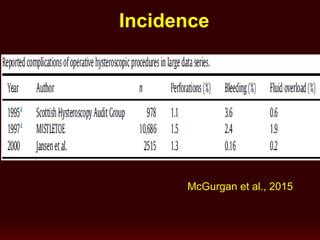
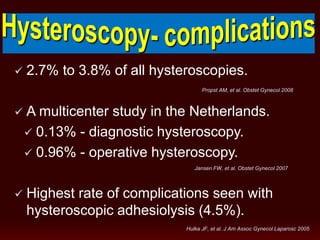
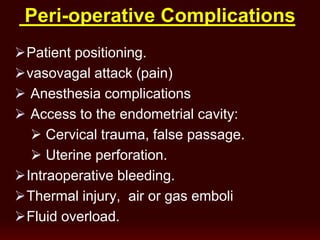
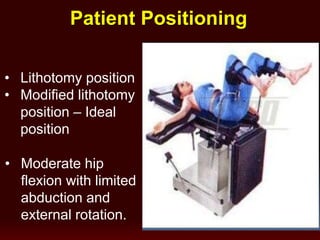
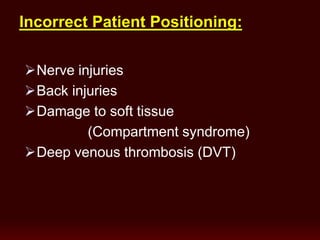
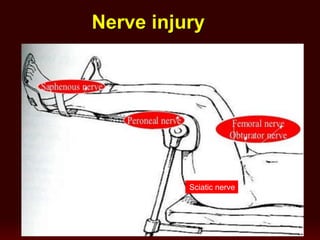
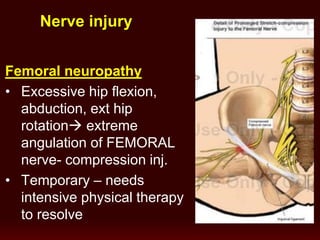
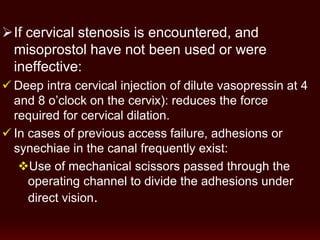
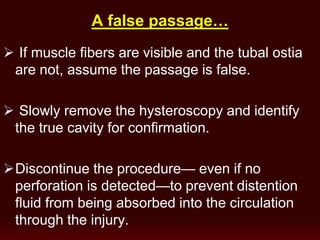
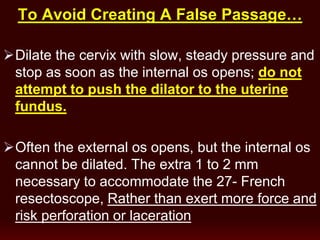
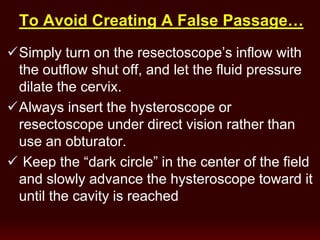
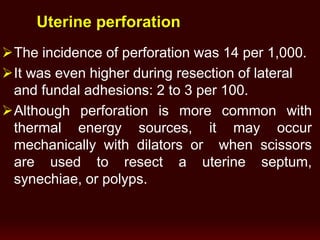
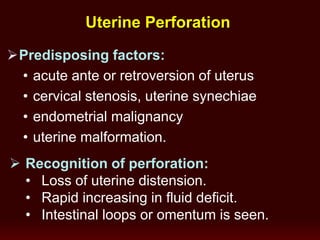
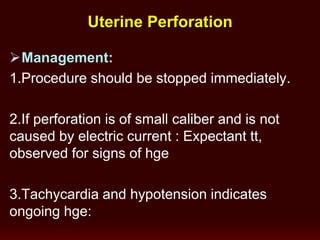
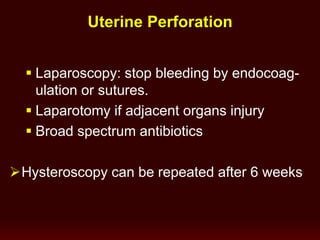
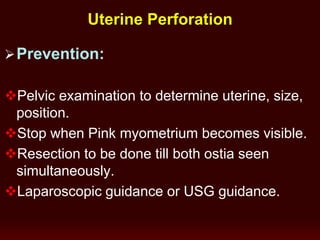
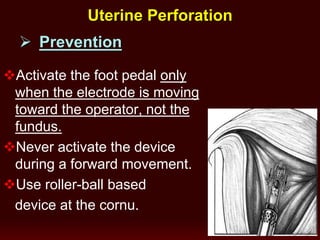
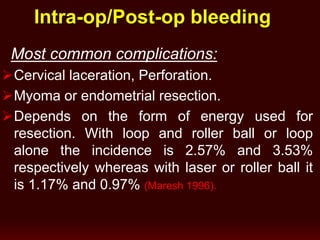
This document discusses complications that can occur during hysteroscopic procedures. It begins by defining various complications such as perforation, bleeding, fluid overload, and infection. It then discusses incidence rates and risk factors for complications. The remainder of the document provides details on specific complications, how to recognize them, and strategies for prevention and management. It emphasizes the importance of proper patient positioning, techniques such as gradual dilation to avoid false passages, and using distension media carefully to prevent fluid overload.




![hemostasisTo achieve
1) Insert a Foley balloon into the uterine cavity,
inflate 30-50 mL (or more for a larger cavity) of
fluid into the balloon, and observe the patient.
The balloon left for 6-12hrs.
2) Pack the uterus.
1/2-inch–gauge packing that has been soaked
in a dilute vasopressin solution.
(20 U [1 mL] in 60 mL Normal Saline).](https://image.slidesharecdn.com/hysteroscopy-complications-170302184120/85/Hysteroscopy-complications-40-320.jpg)
![Benefits of Vasopressin
Before balloon tamponade or Packing the
uterus, Inject very dilute vasopressin :
(4 U [0.2 mL] in 60 mL normal saline)
directly into the cervix 2 cm deep,
at the 4 and 8 o’clock positions.
43](https://image.slidesharecdn.com/hysteroscopy-complications-170302184120/85/Hysteroscopy-complications-42-320.jpg)