Hypothermia and cold injuries are medical conditions that can result from exposure to cold temperatures or freezing conditions. There are three main types discussed:
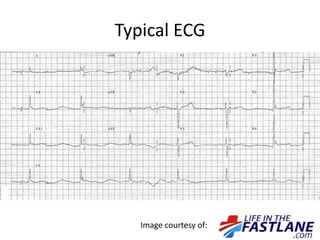
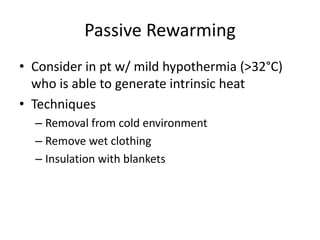
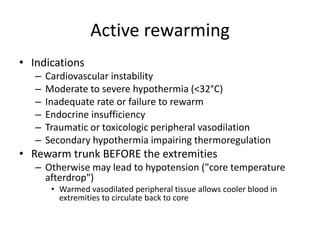
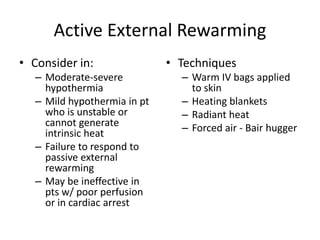
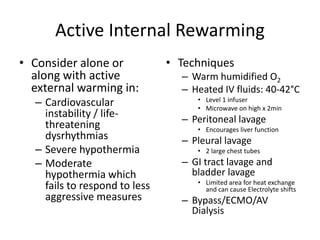
1. Hypothermia is defined as a core body temperature below 35°C and can be mild (32-35°C), moderate (28-32°C), or severe (<28°C) with increasing risks of cardiac dysrhythmias and arrest. Rewarming methods include passive rewarming for mild cases or active external and internal rewarming for more severe hypothermia.
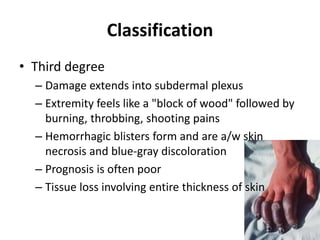
2. Frostbite causes freezing of the skin and deeper tissues, classified into 4 degrees of injury ranging from superficial frostnip to deep tissue freezing and