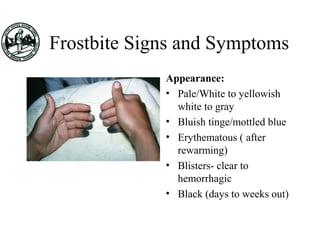
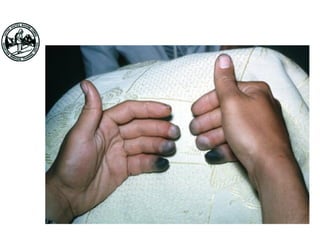
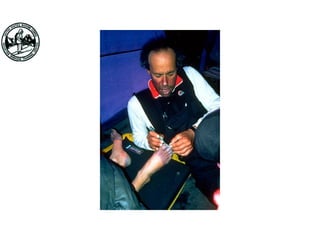
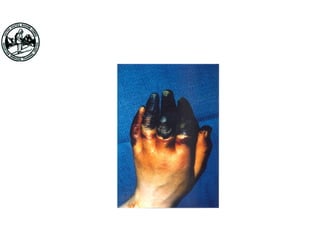
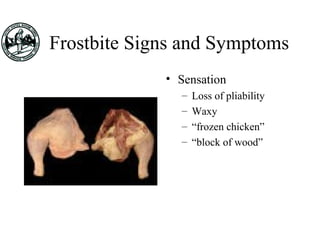
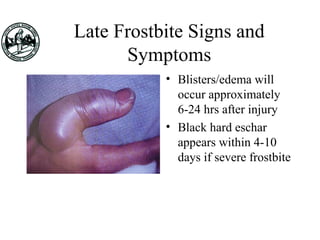
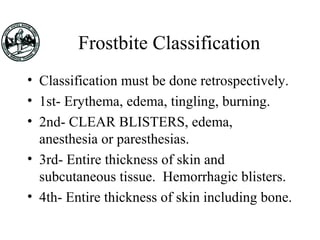
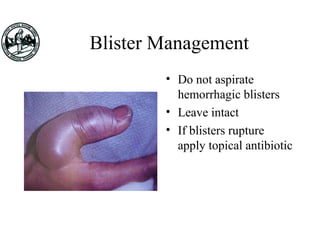
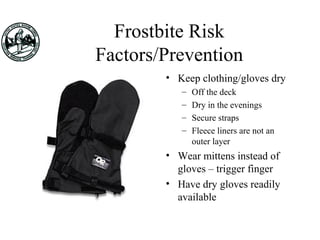
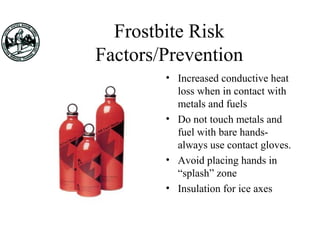
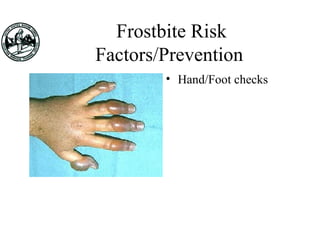
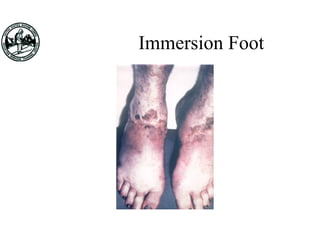
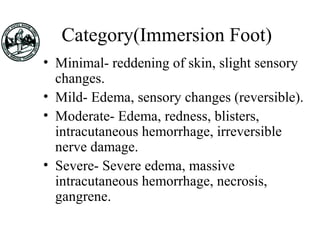
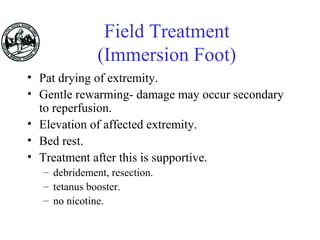
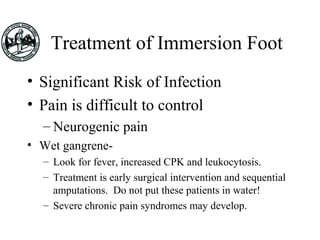
Frostbite and immersion foot are cold injuries caused by prolonged exposure to wet and cold conditions. Frostbite results from actual freezing of tissue and causes numbness, pain, blistering and tissue death. Treatment involves rapid rewarming in warm water followed by pain medication and wound care. Immersion foot occurs in wet, non-freezing environments and causes swelling, blistering and nerve damage. Prevention of both injuries focuses on keeping skin dry and body insulated through proper clothing, activity, hydration and avoiding nicotine use.