This document discusses hypothermia and frostbite. Some key points:
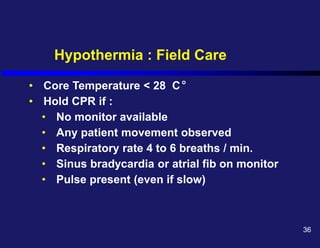
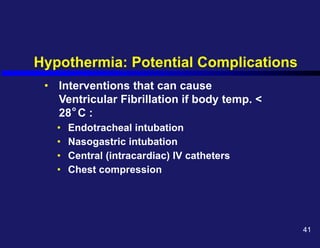
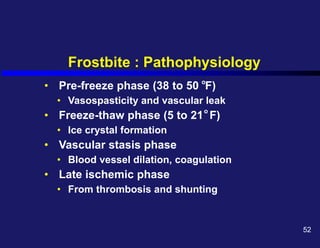
1. Hypothermia is defined as a body temperature below 35°C (95°F). Severe hypothermia is below 28°C. It can cause confusion, loss of consciousness, and death.
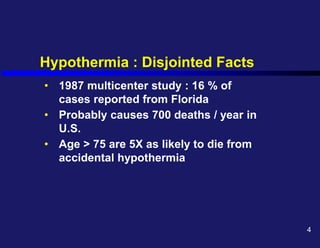
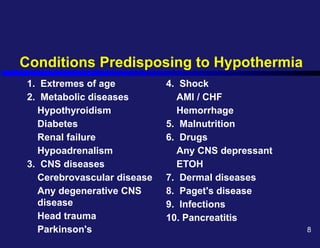
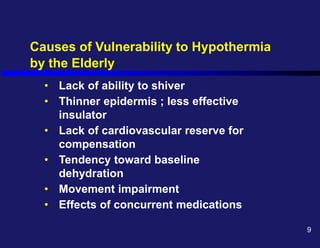
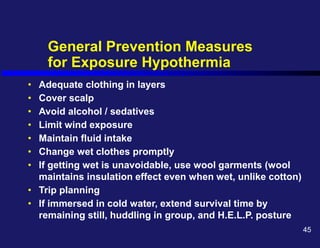
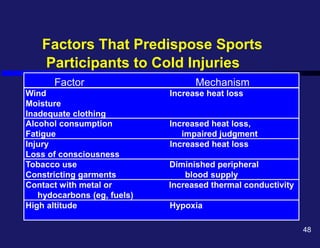
2. Risk factors for hypothermia include extremes of age, medical conditions, drugs/alcohol, malnutrition, and exposure to cold. The elderly are especially vulnerable due to thinner skin and reduced ability to shiver.
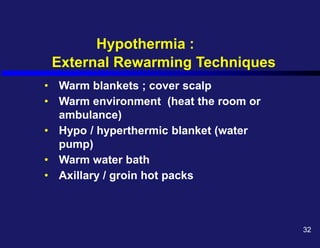
3. Rewarming techniques include warmed oxygen, IV fluids, gastric/rectal lavage, and external warming. The goal is to raise the core temperature over 1°C