This document provides an overview of Graves' disease. It discusses the epidemiology, pathophysiology, clinical manifestations, diagnostic evaluation and treatment options. The key points are:
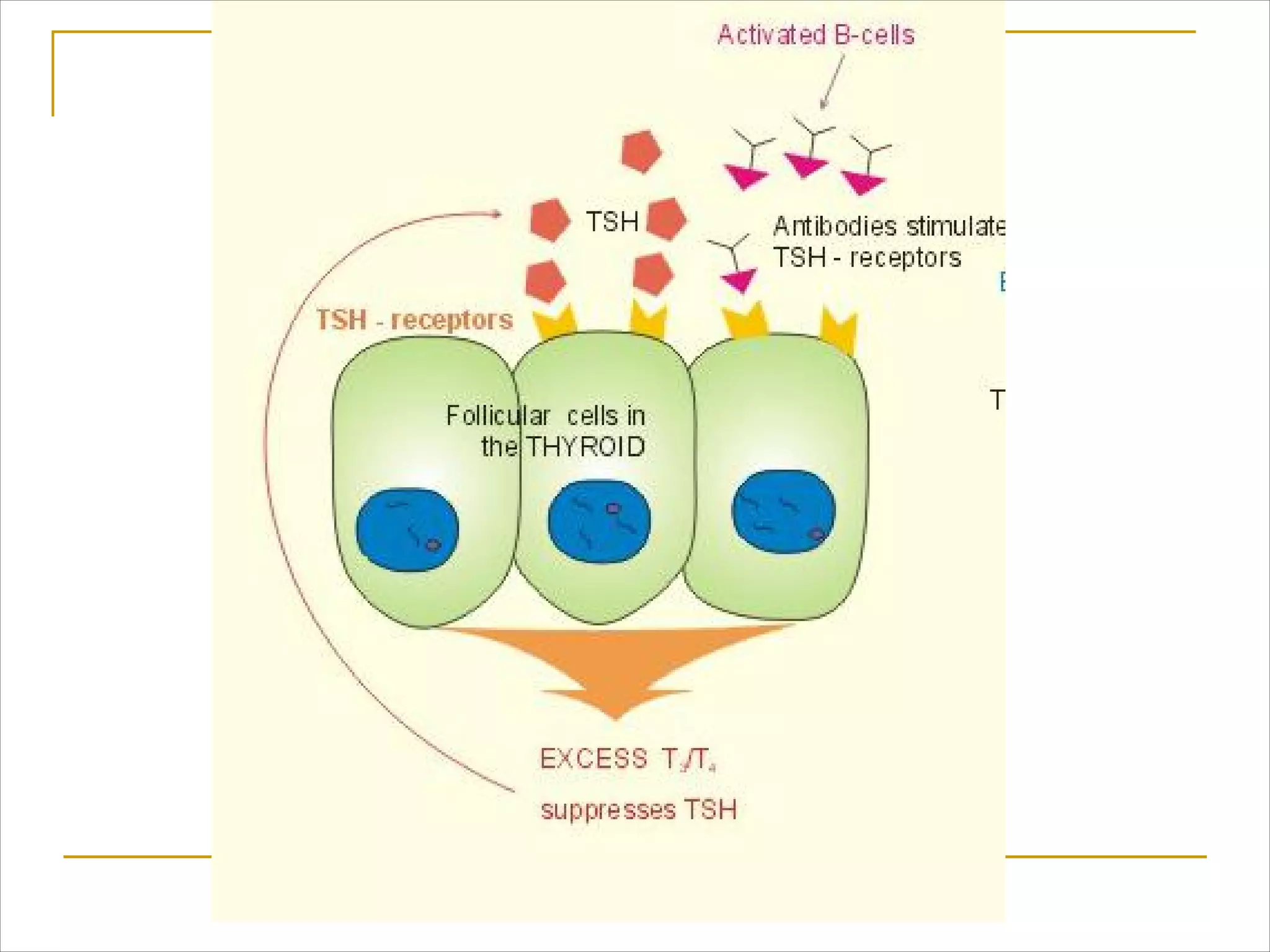
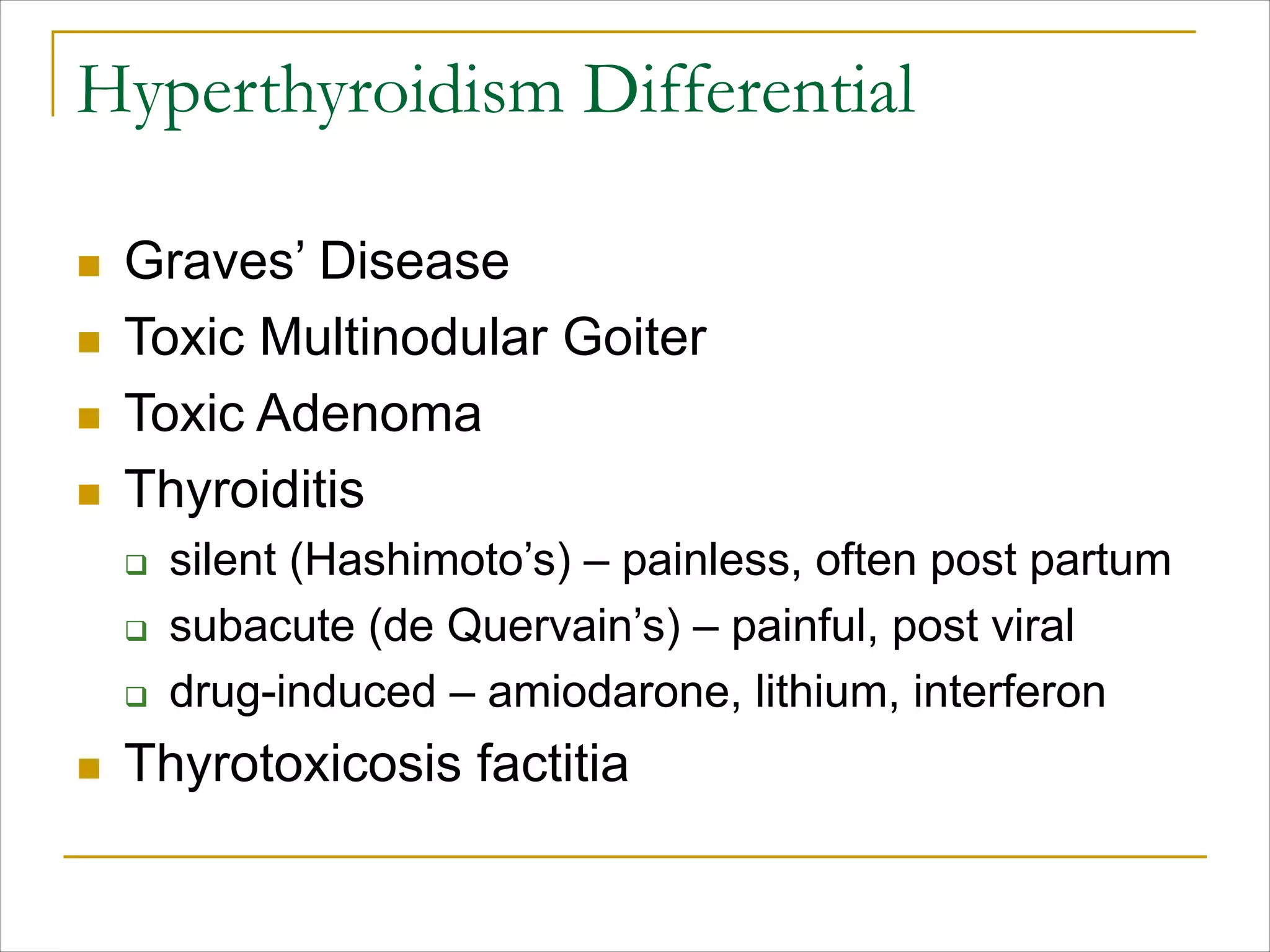
- Graves' disease is the most common cause of hyperthyroidism and is an autoimmune disorder causing the thyroid to produce too much hormone.
- It commonly affects women ages 30-50 and presents as thyrotoxicosis with or without a goiter.
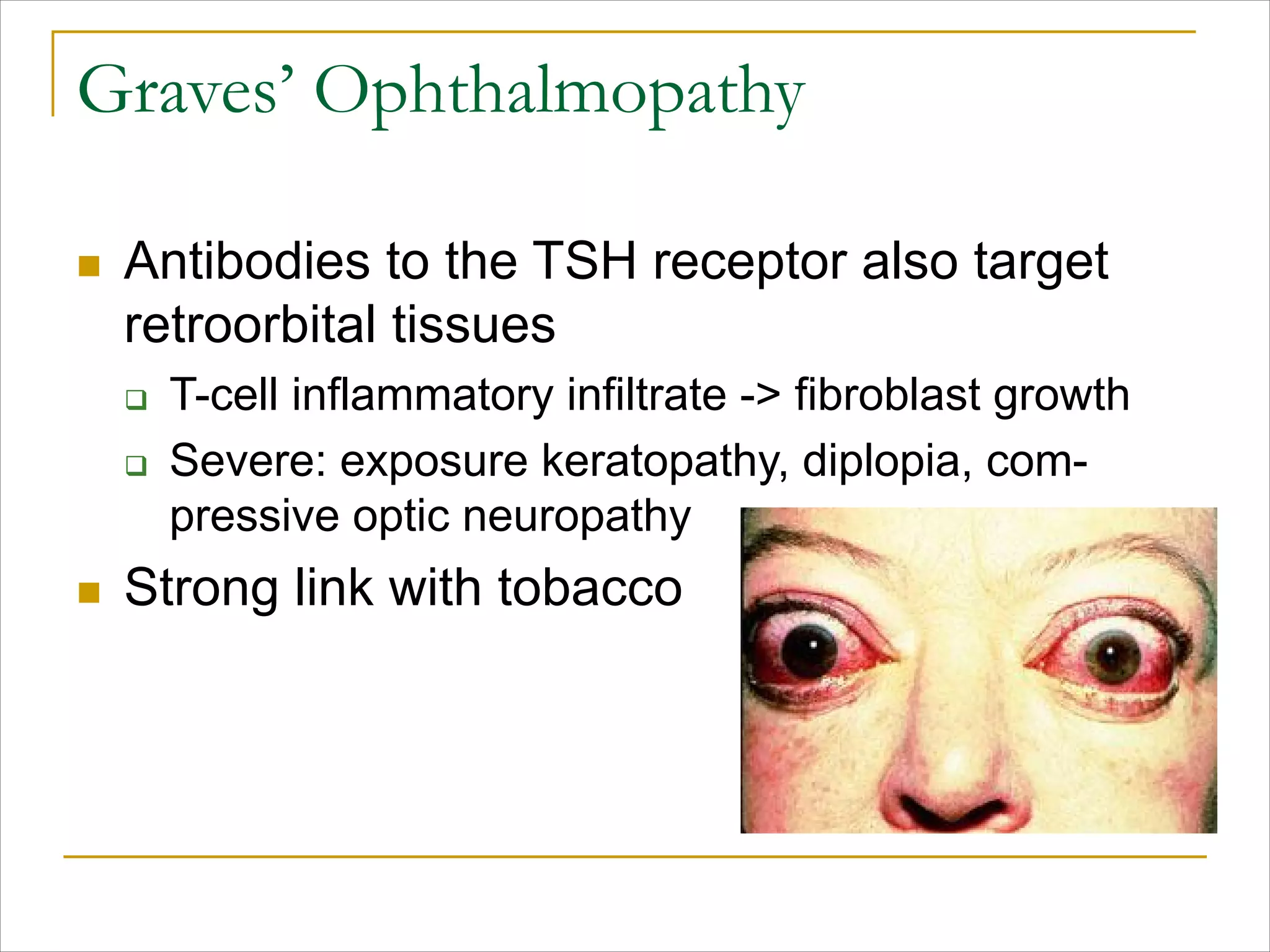
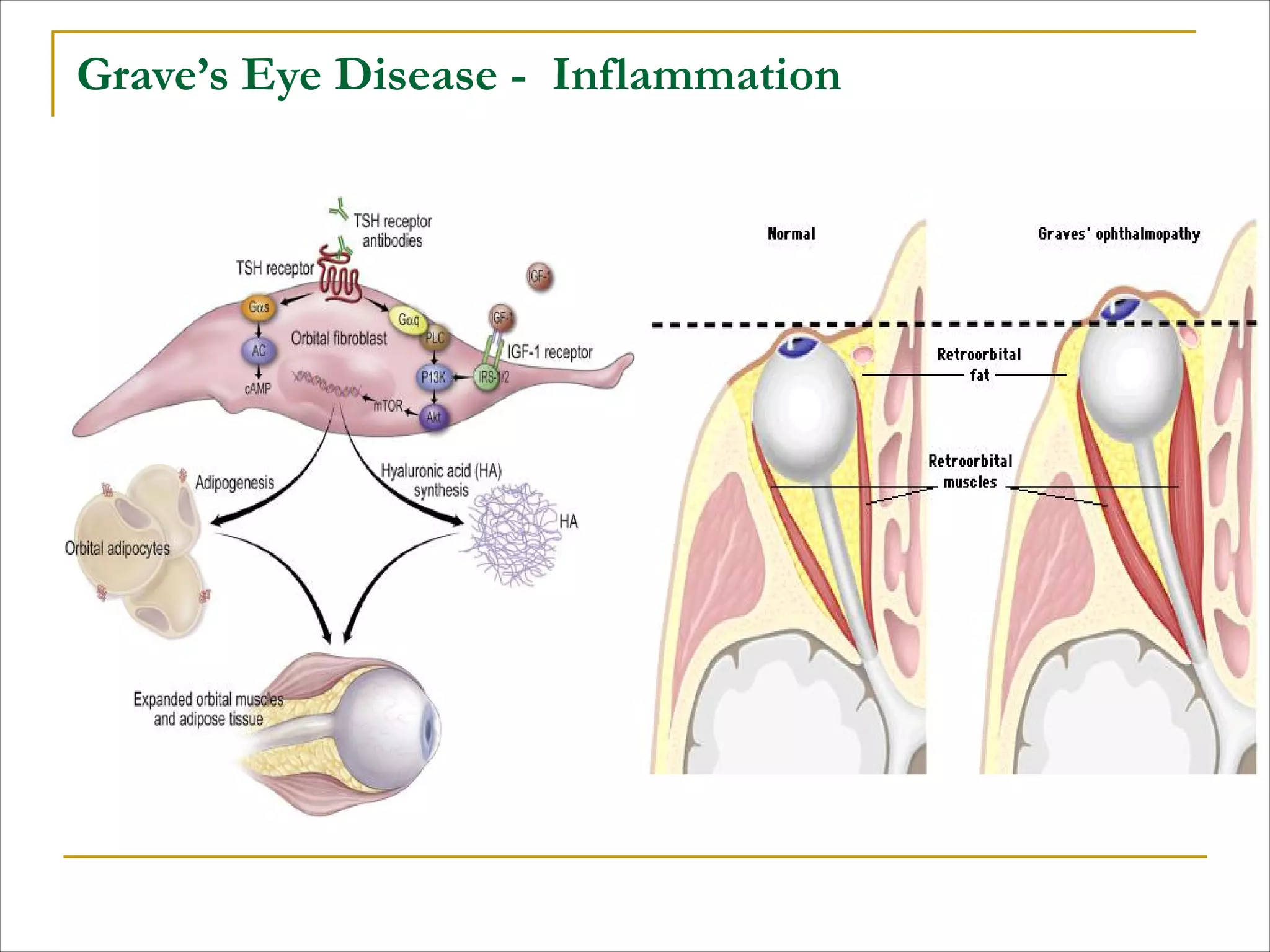
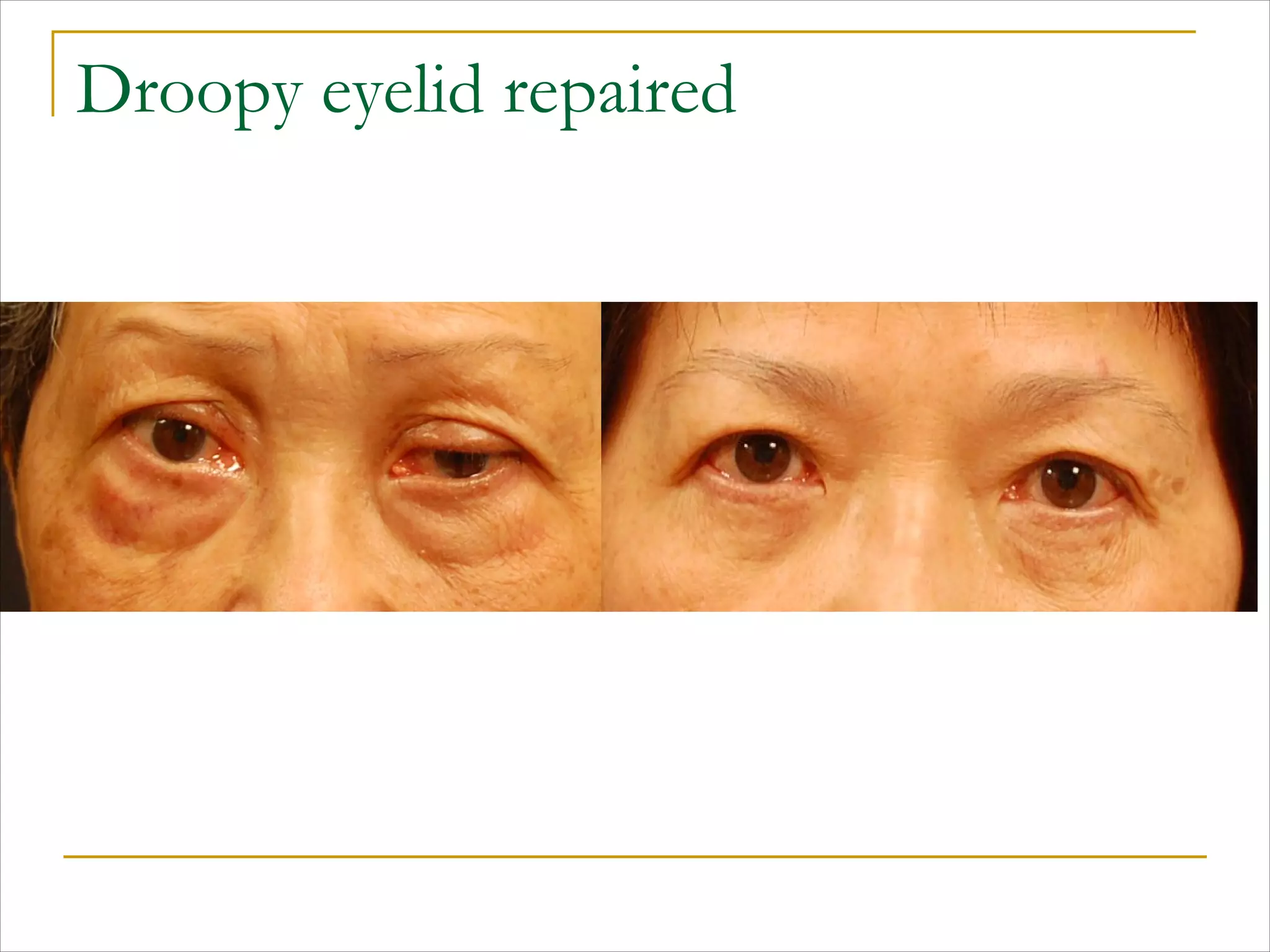
- Clinical manifestations include hyperthyroidism, ophthalmopathy in 20-40% of cases, and dermopathy in rare cases.
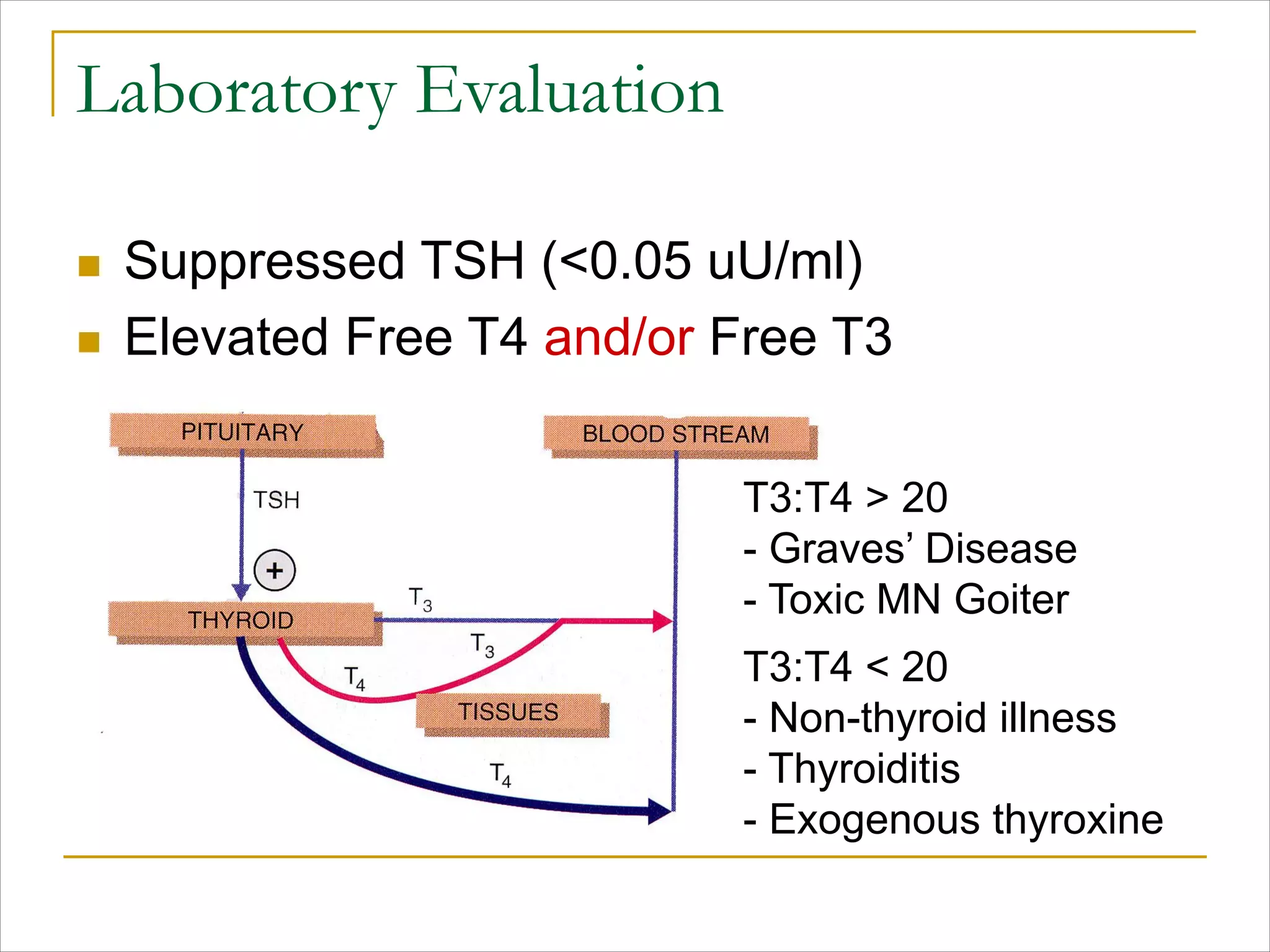
- Diagnosis involves lab tests showing suppressed TSH and elevated T3/T4, and imaging may include ultrasound