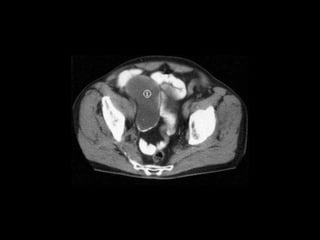
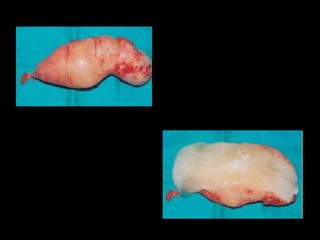
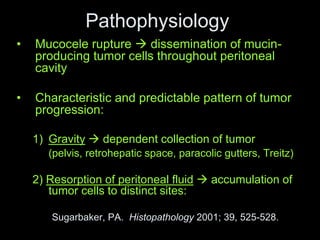
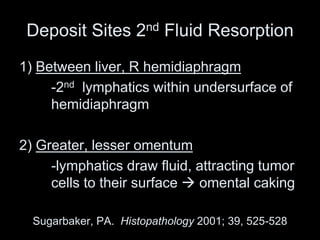
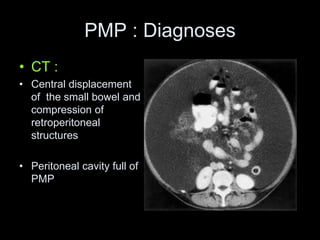
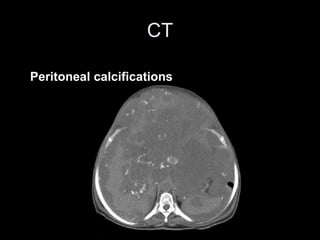
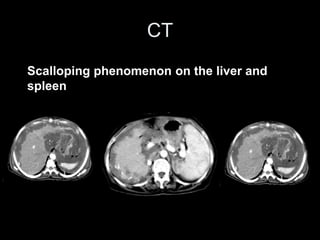
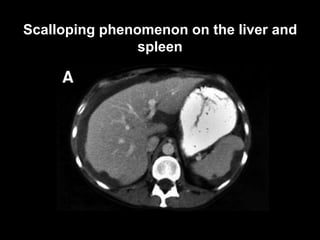
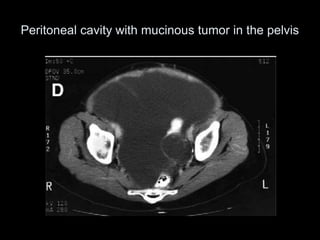
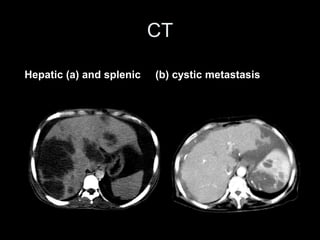
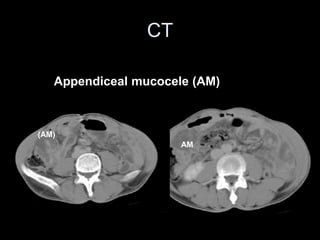
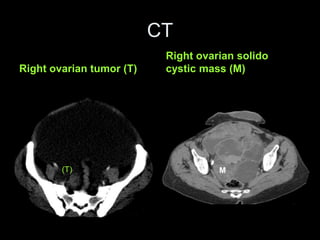
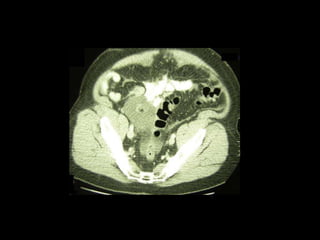
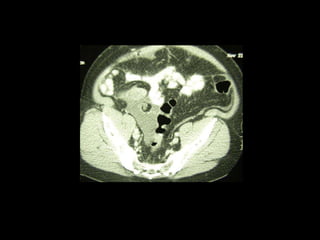
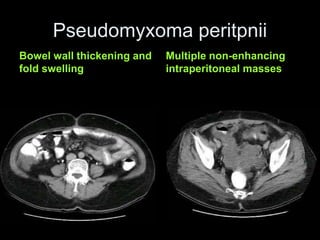
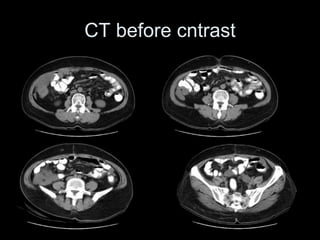
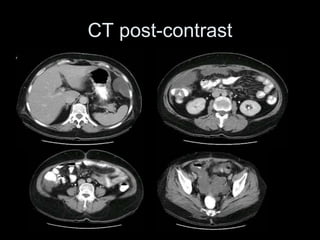
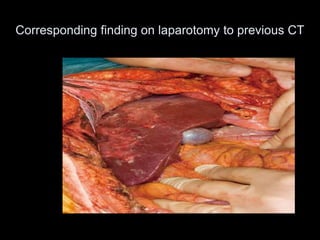
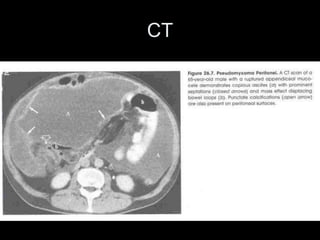
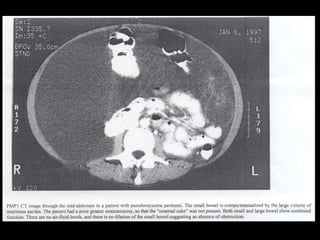
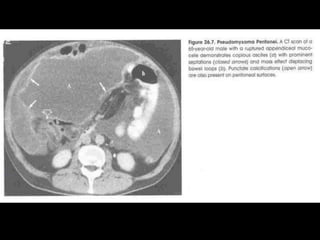
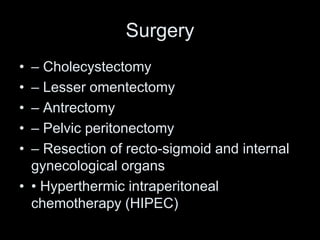
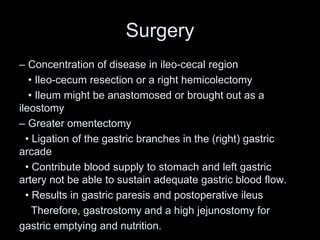
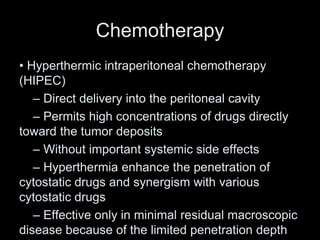
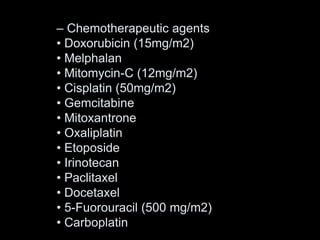
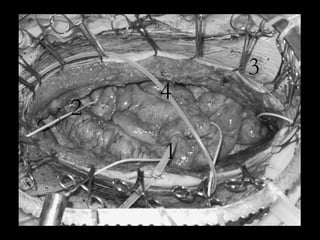
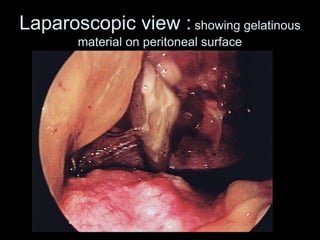
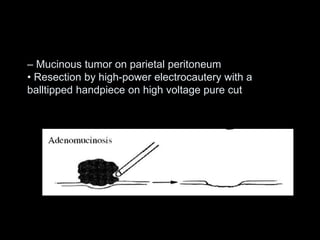
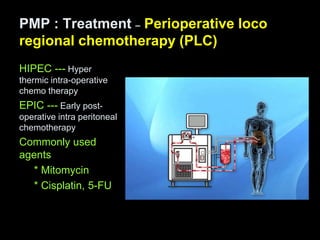
Pseudomyxoma peritonei is a rare disease characterized by diffuse gelatinous ascites and mucinous tumor implants throughout the peritoneal cavity. It is usually caused by the rupture of a mucin-producing tumor, often originating from the appendix. Diagnosis is typically made through CT imaging and surgical exploration. Treatment involves aggressive cytoreductive surgery to remove all visible tumor deposits combined with hyperthermic intraperitoneal chemotherapy to address any remaining microscopic disease. This multimodal approach has improved long-term survival rates compared to surgery alone, with some reports of 80% 10-year survival when all tumor nodules can be completely resected.