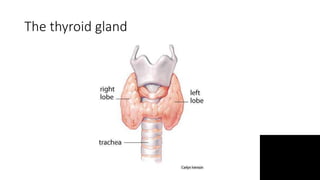
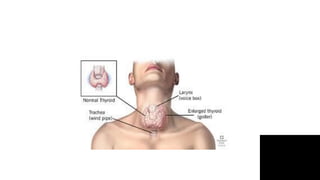
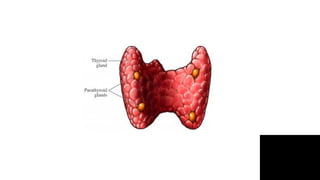
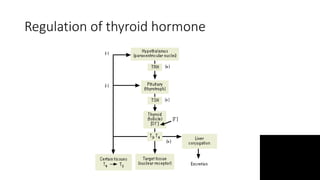
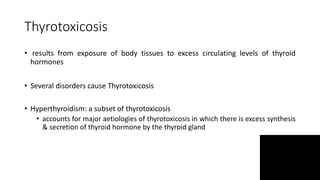
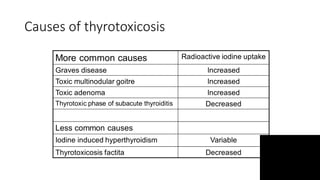
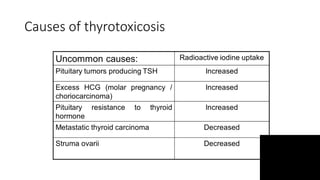
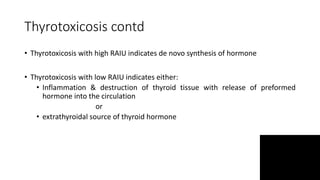
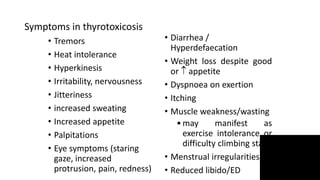
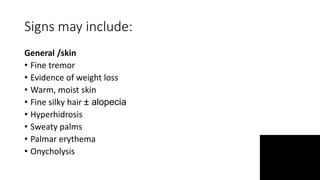
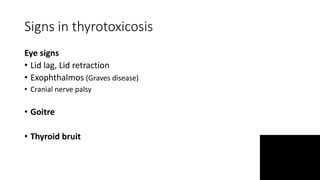
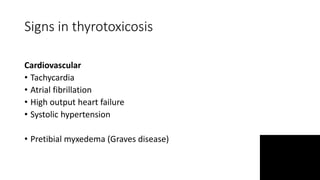
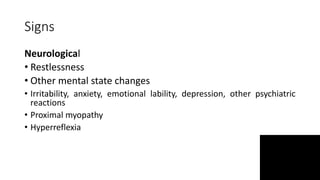
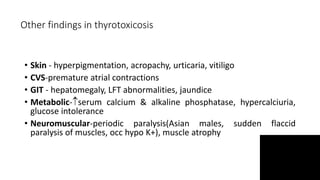
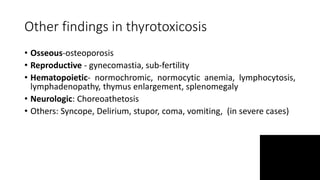
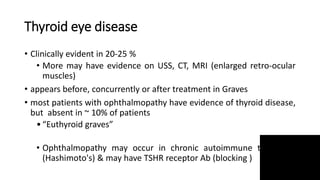
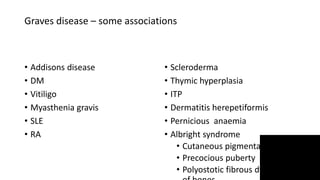
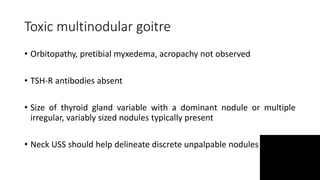
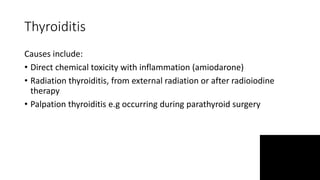
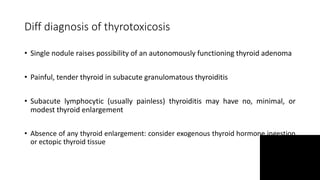
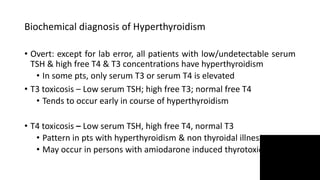
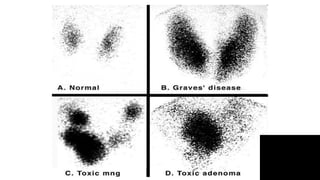
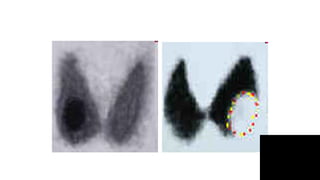
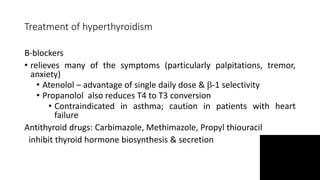
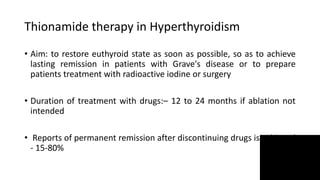
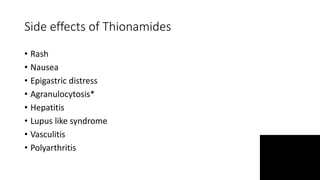
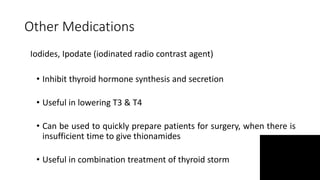
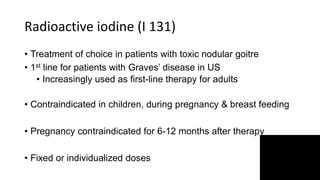
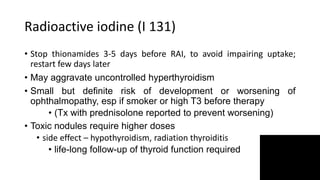
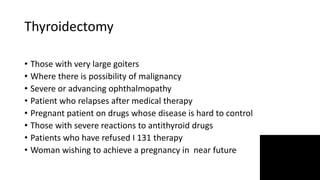
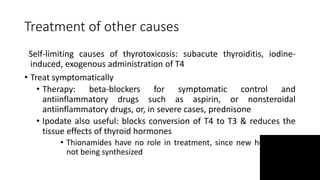
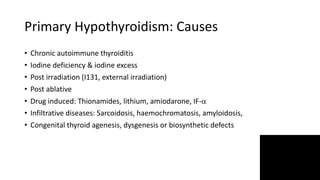
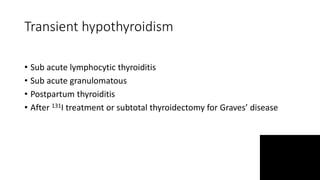
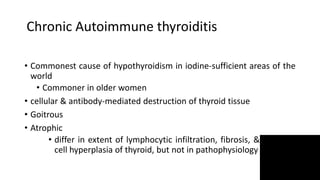
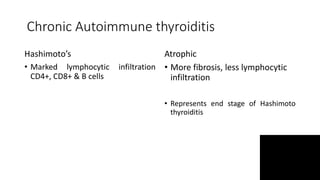
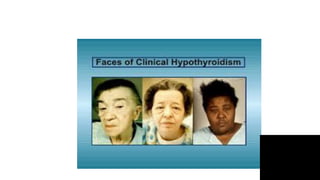
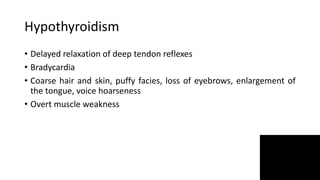
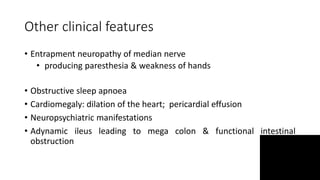
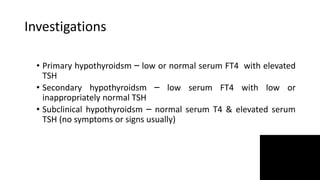
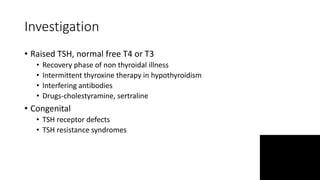
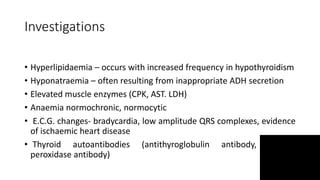
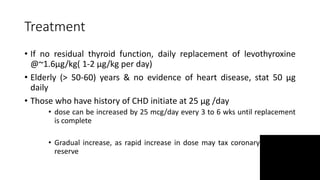
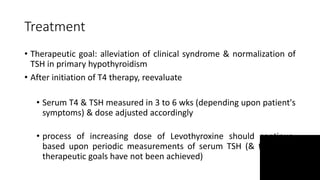
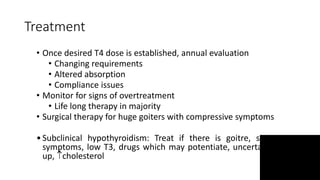
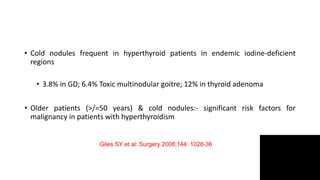
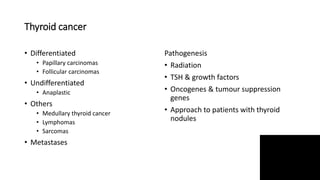
Thyroid disorders are common in endocrinology. The document discusses the anatomy and functions of the thyroid gland, as well as the regulation of hormone production and classification of thyroid disorders. It provides an overview of hyperthyroidism (thyrotoxicosis) and hypothyroidism, including their causes, signs, symptoms, and treatment approaches. Graves' disease is described as the most common cause of thyrotoxicosis. Treatment options for hyperthyroidism discussed include beta-blockers, antithyroid medications, radioactive iodine, and thyroidectomy.