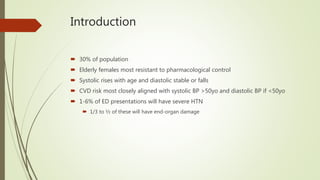
This document discusses systemic hypertension, including:
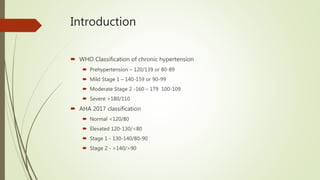
- Definitions of different classifications of hypertension according to WHO and AHA guidelines.
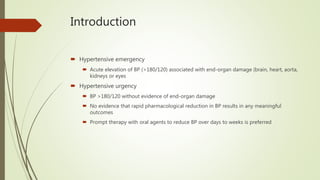
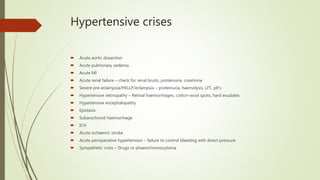
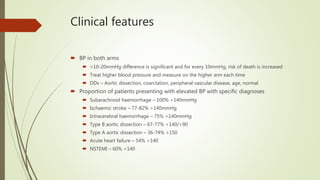
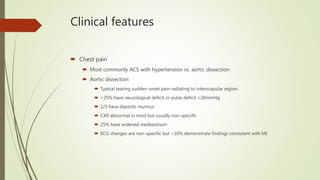
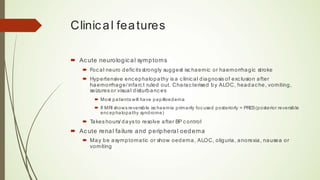
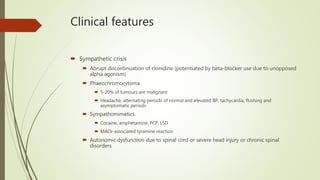
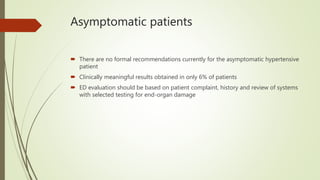
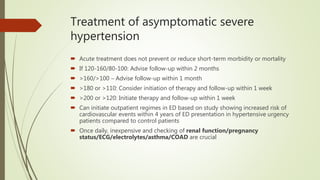
- Differences between hypertensive emergencies and urgencies.
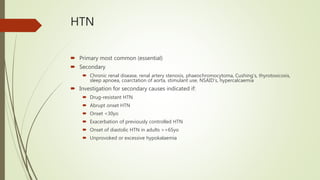
- Common causes and clinical presentations of secondary hypertension.
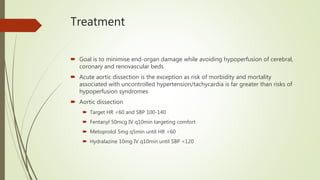
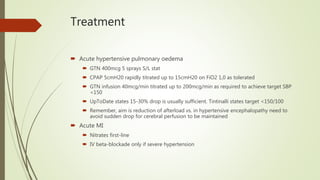
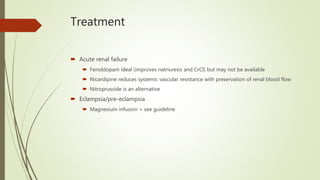
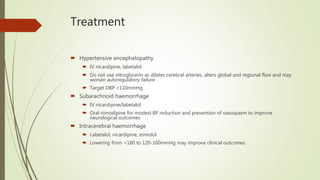
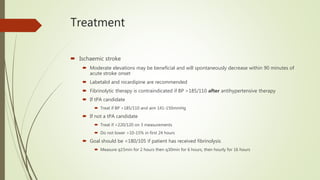
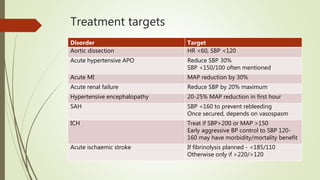
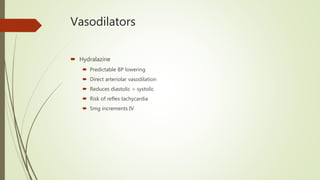
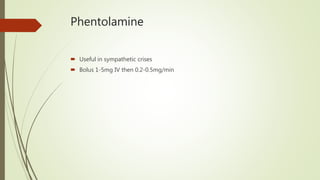
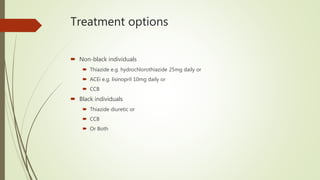
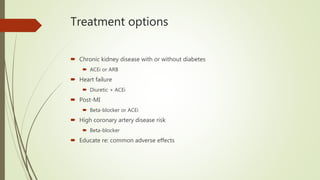
- Recommended treatment approaches for various hypertensive crises and emergencies, including targets for blood pressure reduction.
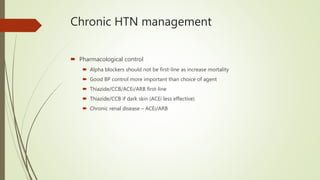
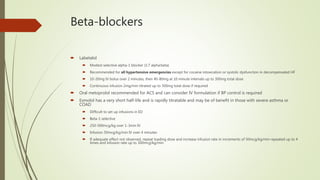
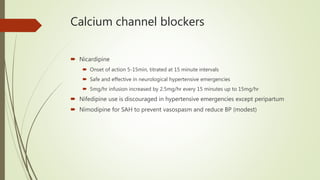
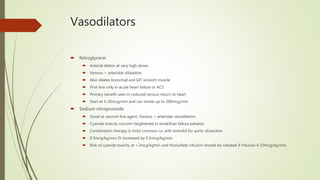
- Drugs commonly used to lower blood pressure such as labetalol, nicardipine, nitroglycerin, and sodium nitroprusside.