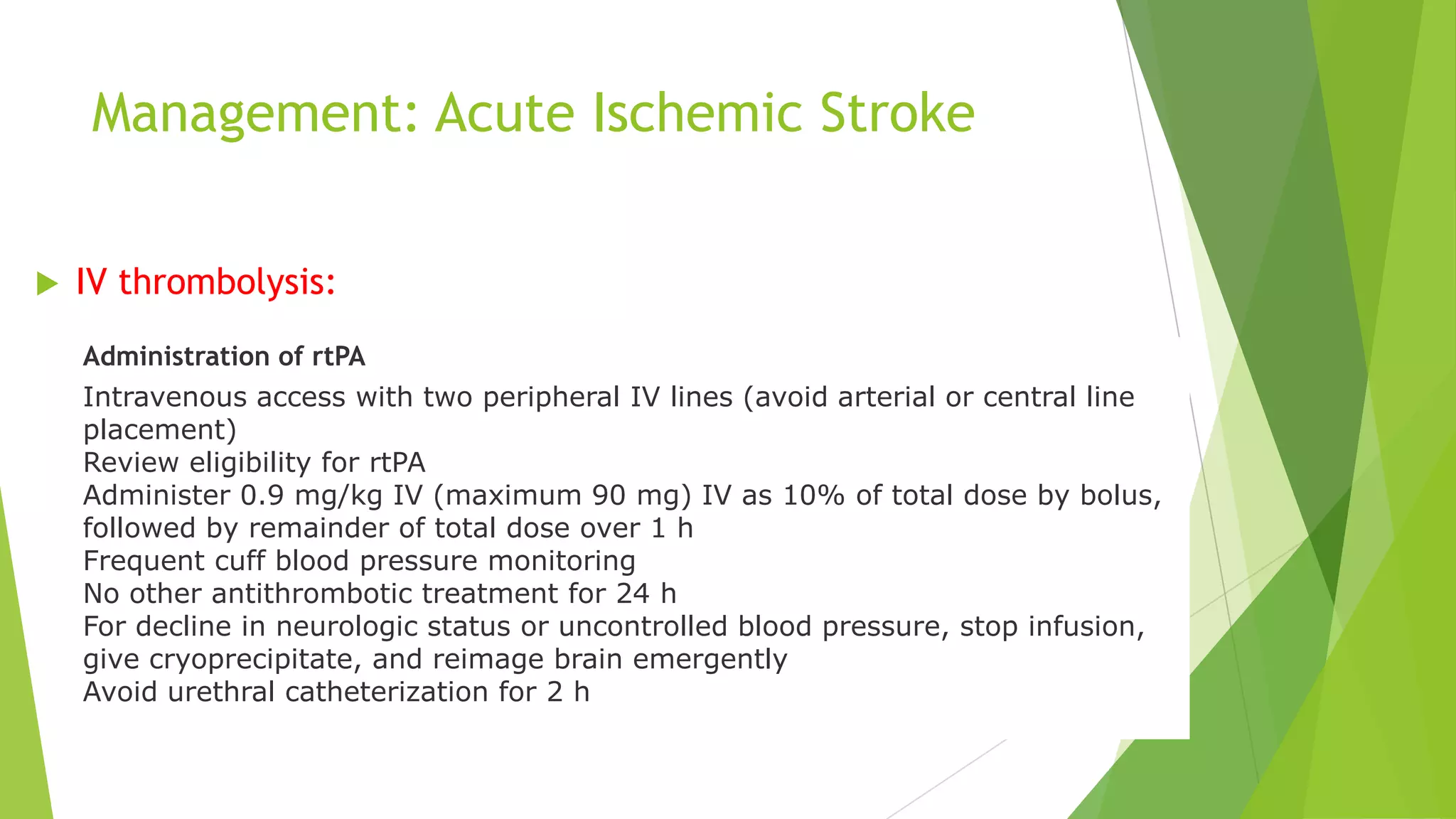
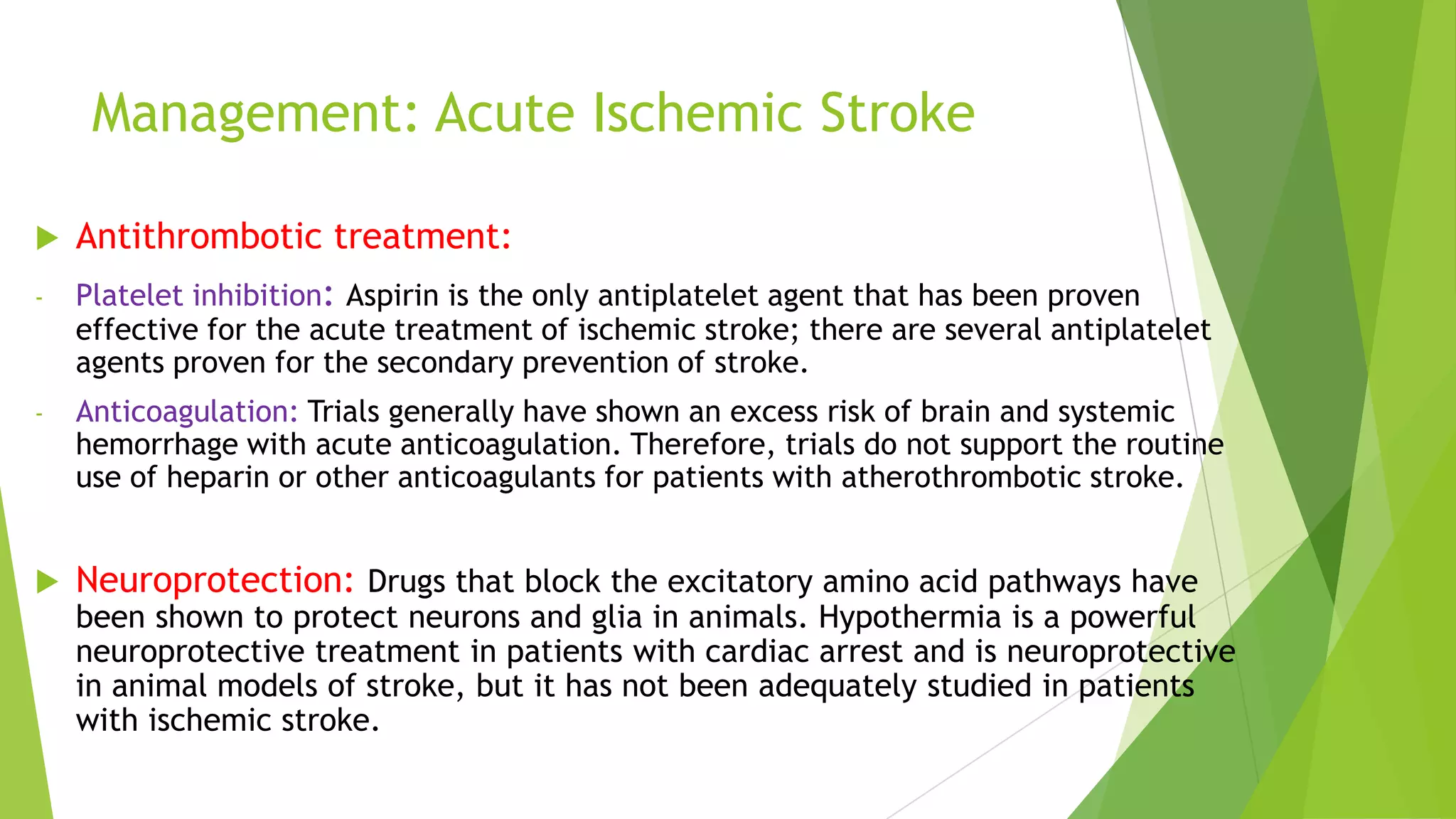
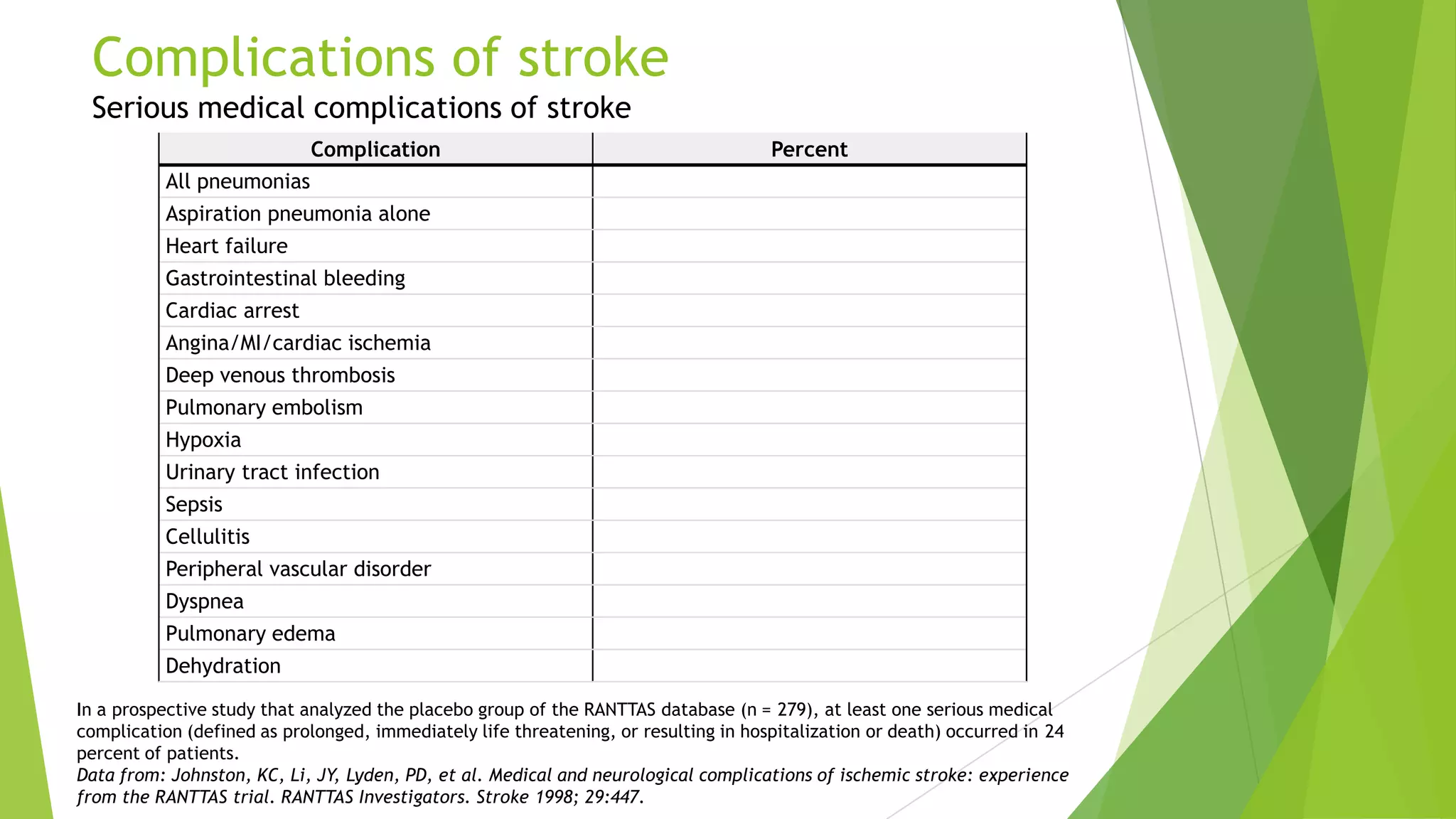
This document summarizes the management and complications of stroke. It discusses the medical management of acute ischemic stroke, which falls into six categories: medical support, IV thrombolysis, endovascular techniques, antithrombotic treatment, neuroprotection, and stroke centers and rehabilitation. It also outlines common complications of stroke seen in studies such as falls, urinary tract infections, chest infections, pressure sores, and depression. Serious complications discussed include various types of pneumonia, heart failure, gastrointestinal bleeding, cardiac arrest, and deep venous thrombosis.