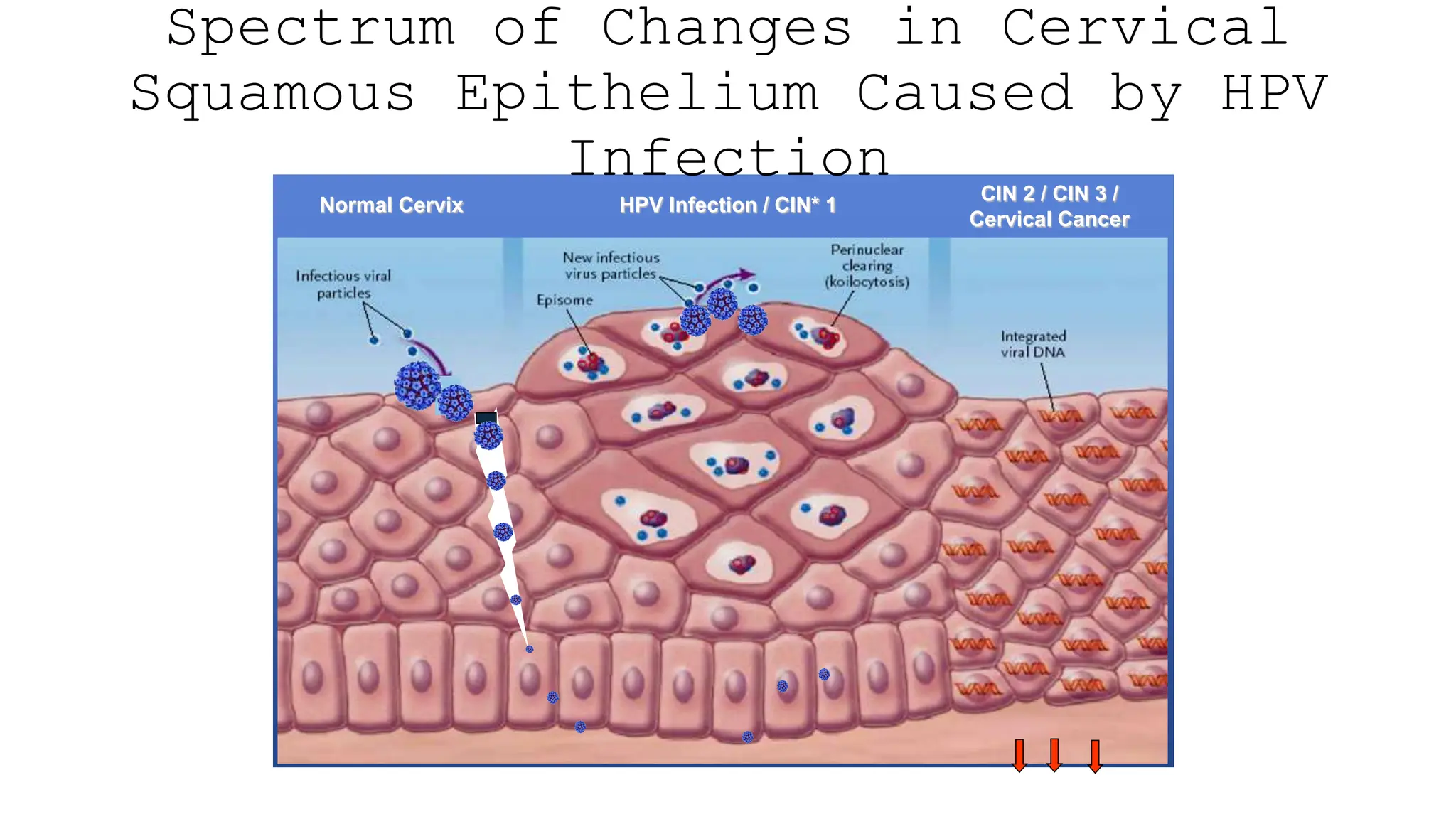
Cervical cancer, attributed mainly to HPV, is a significant health concern, ranking as the fourth most common cancer among women globally, with preventive measures like HPV vaccination and screening showing promise in reducing incidence. The WHO's cervical cancer elimination strategy aims to achieve a target incidence of 4/100,000 women by 2030 through vaccination, screening, and treatment plans. Treatment options vary based on the stage of cancer, with emphasis on conservative approaches for early-stage disease and combined therapies for advanced cases.