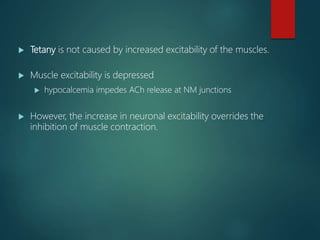
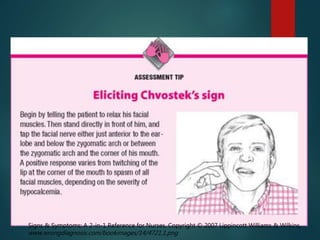
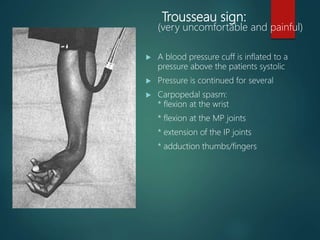
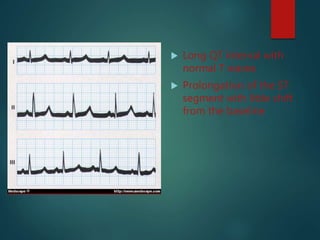
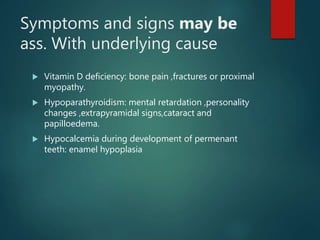
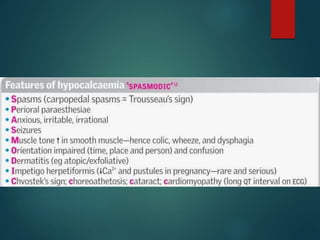
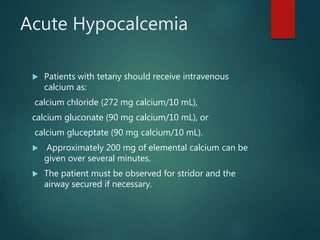
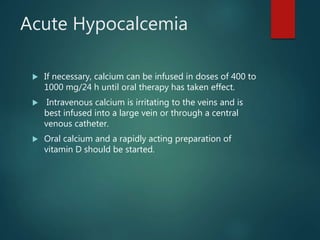
Hypocalcemia is a low level of calcium in the blood. Calcium is essential for nerve impulse conduction, muscle contraction, and other cellular functions. Hypocalcemia can be caused by low albumin, low parathyroid hormone, vitamin D deficiency, or other factors. Symptoms include neuromuscular irritability, tetany, seizures, and EKG changes. Treatment involves oral calcium and vitamin D supplements to replace calcium and maintain adequate blood levels. Intravenous calcium may be needed for severe acute hypocalcemia.
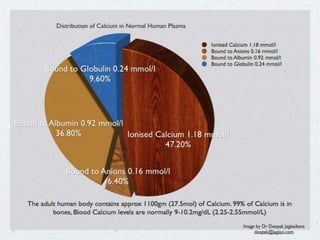
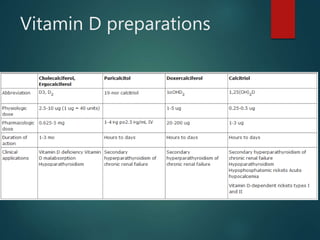
![Hypoalbuminemia
produces a low total serum [Ca2+] because of a
reduction in the bound fraction of calcium, but the
ionized [Ca2+] is normal. The ionized [Ca2+] can be
determined directly, or the effect of hypoalbuminemia
can be roughly corrected for by using the following
formula:
Corrected serum calcium = Measured serum calcium +
(0.8) (4 – Measured serum albumin)
Thus, in a patient with a serum [Ca2+] of 7.8 mg/dL and
a serum albumin of 2 g/dL, the corrected serum [Ca2+]
is 7.8 + (0.8)(4 – 2) = 9.4 mg/dL.](https://image.slidesharecdn.com/hpocalcemia-160930041338/85/Hpocalcemia-7-320.jpg)





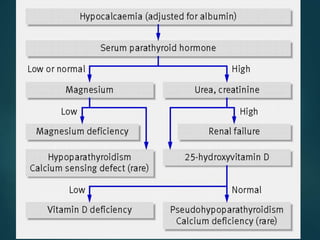
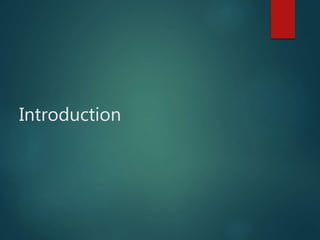
![Chronic Hypocalcemia
The aim of chronic therapy is to: keep the patient free
of symptoms and to maintain a serum [Ca2+] of
approximately 8.5 to 9.0 mg/dL.
With lower serum [Ca2+], the patient may not only
experience symptoms but may be predisposed over
time to cataract formation if the phosphate level is also
high.](https://image.slidesharecdn.com/hpocalcemia-160930041338/85/Hpocalcemia-33-320.jpg)