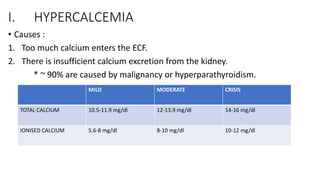
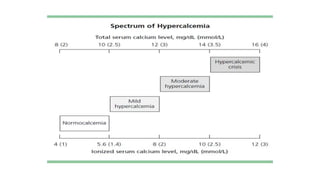
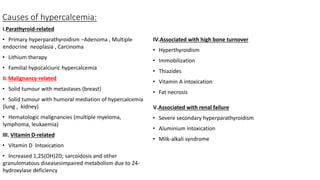
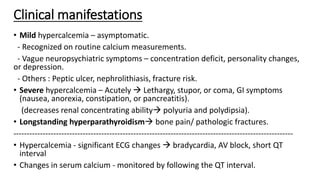
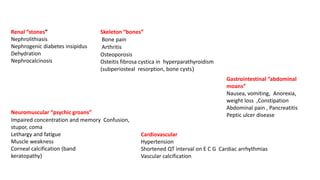
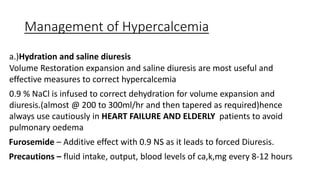
This document discusses hypercalcemia and hypocalcemia, including their causes, symptoms, and management. Hypercalcemia can be caused by hyperparathyroidism, certain malignancies, vitamin D toxicity, and other conditions. Symptoms range from none in mild cases to fatigue, nausea, and cognitive issues in severe cases. Treatment focuses on rehydration, bisphosphonates, calcitonin, surgery, and addressing the underlying cause. Hypocalcemia is usually asymptomatic but can cause tingling and seizures in severe cases. It is often caused by hypoparathyroidism, vitamin D deficiency, or tumor lysis syndrome. Treatment involves calcium and vitamin D supplementation to address the deficiency. Laboratory tests are important to
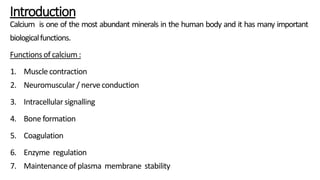
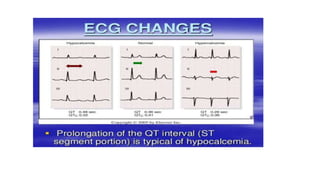
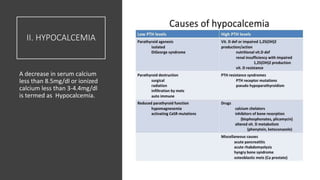
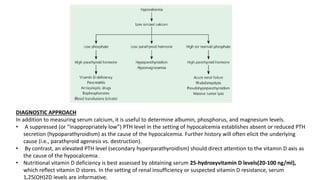
![Calculation of calcium levels:
• Step1:Ensurethatthealterationinserumcalciumlevelsisnotduetoabnormal
albuminconcentration(sinceionizedformistheactiveformofcalcium)
• Directmeasurementof ionisedcalciumiseasilyinfluencedbycollection
methodsandotherartefacts,hencewe prefertomeasurecorrectedcalcium
fromtotalcalciumandalbumin.
Corrected calcium:
• For every 1-g/dL drop in serum albumin below 4 g/dL, measured serum calcium
decreasesby0.8 mg/dL.
• Correctedcalcium=MeasuredCa+[0.8x(4–measuredalbumin)]
(Calciuminmg/dl;albumining/dl)](https://image.slidesharecdn.com/gowthams1st-190115074354/85/Hyper-and-hypocalcemia-4-320.jpg)
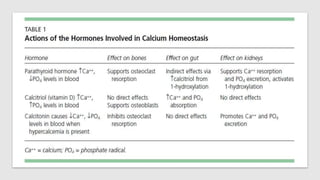
![TUMOUR LYSIS SYNDROME
• Tumor cell death with the release of intracellular
contents can lead to a constellation of metabolic
abnormalities is tumor lysis syndrome (TLS).
• it can occur spontaneously in rapidly proliferating
tumors, it occurs most frequently following
administration of cytotoxic chemotherapy to patients
with hematologic malignancies, with a large percentage
of proliferating, drug-sensitive cells . Ex: acute leukemias
,large bulky high-grade non-Hodgkin lymphomas [NHL],
especially Burkitt lymphoma
• TLS occurs a few hours to a few days after the initiation
of therapy.
• Cell death leads to the release of potassium, phosphate,
uric acid, and other purine metabolites overwhelming
the kidney’s capacity for clearance with resultant
hyperkalemia, hyperphosphatemia and secondary
hypocalcemia, and hyperuricemia
• Unchecked, TLS can progress to acute renal failure and
metabolic acidosis . Established TLS is associated with a
high morbidity and mortality.
Cairo Bishop classification system](https://image.slidesharecdn.com/gowthams1st-190115074354/85/Hyper-and-hypocalcemia-21-320.jpg)
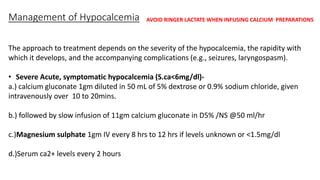
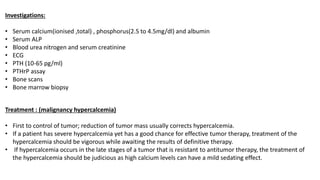
![• Moderate hypocalcemia: (6-8 mg/dl)
a.) calcium either oral or IV (1000mg of elemental iron daily)
b.) magnesium 1gm IV once/twice daily
c.) patients recovering from hypercalcemia are in risk
• Chronic hypocalcemia due to hypoparathyroidism is treated with calcium
supplements (1000–1500 mg/d elemental calcium in divided doses) and either
vitamin D2 or D3 (25,000–100,000 U daily) or calcitriol [1,25(OH)2D, 0.25–2
μg/day].
• Vitamin D deficiency, however, is best treated using vitamin D supplementation,
with the dose depending on the severity of the deficit and the underlying cause.](https://image.slidesharecdn.com/gowthams1st-190115074354/85/Hyper-and-hypocalcemia-26-320.jpg)