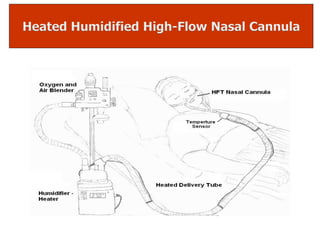
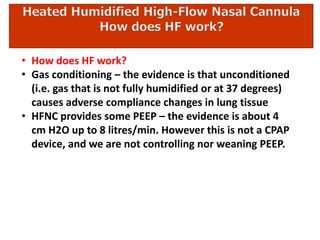
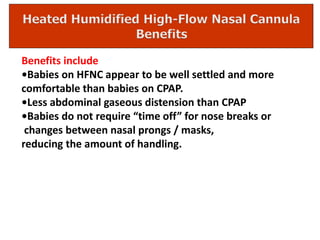
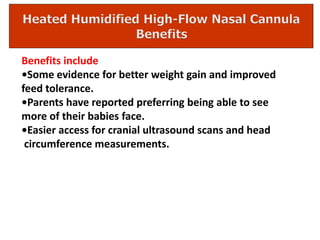
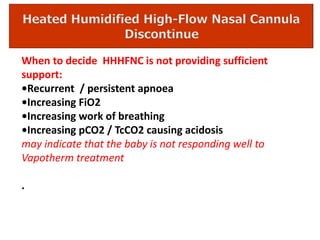
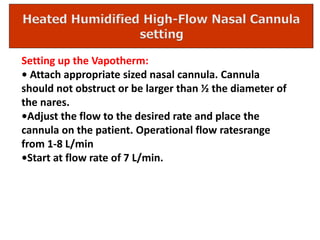
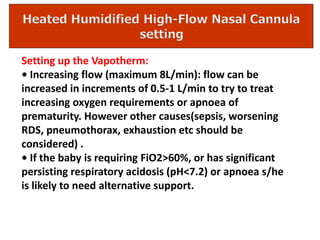
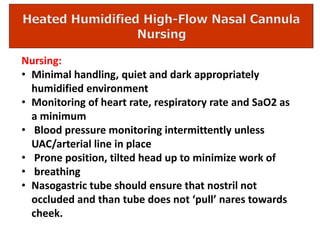
Heated, humidified high-flow nasal cannula (HHHFNC) is commonly used as a noninvasive mode of respiratory support in the NICU to avoid prolonged ventilator support and ventilator-induced lung injury. HHHFNC delivers humidified heated and blended oxygen/air at flow rates greater than 1L/min via nasal cannula. The mechanisms of how HHHFNC works include flushing out the nasal airway, providing some positive end-expiratory pressure, and conditioning the gas. Benefits of HHHFNC include improved comfort for babies, less abdominal distension than CPAP, and easier access for procedures. HHHFNC is considered insufficient support if a baby has