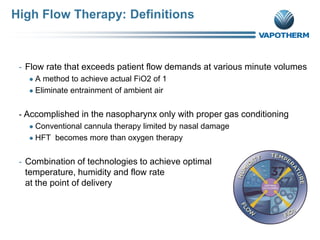
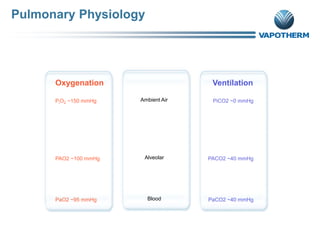
This document provides an overview of high flow therapy (HFT) in the neonatal population and the Precision Flow system. It discusses the clinical review of HFT, including definitions, mechanisms of action like humidifying/warming airways and flushing dead space. It also reviews the Precision Flow system, including its overview, features, and disposable patient circuit components like the vapor transfer cartridge. Indications for HFT include spontaneously breathing patients requiring oxygen therapy or post-extubation support. The document aims to demonstrate how HFT provides several benefits over conventional oxygen therapy through various physiological mechanisms.