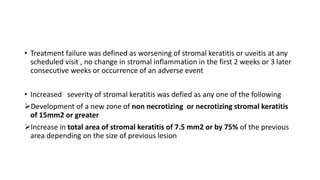
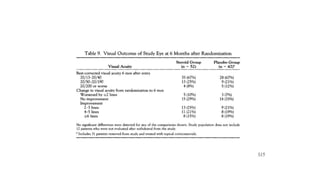
This document summarizes a randomized controlled trial that evaluated the efficacy of topical corticosteroids for treating herpes simplex stromal keratitis. The trial involved 106 patients who were randomly assigned to receive either topical prednisolone phosphate plus trifluridine or placebo plus trifluridine. Patients receiving corticosteroids were less likely to have treatment failure and had faster resolution of stromal keratitis. The use of corticosteroids with antiviral cover was found to be effective for acute treatment of herpes simplex stromal keratitis.