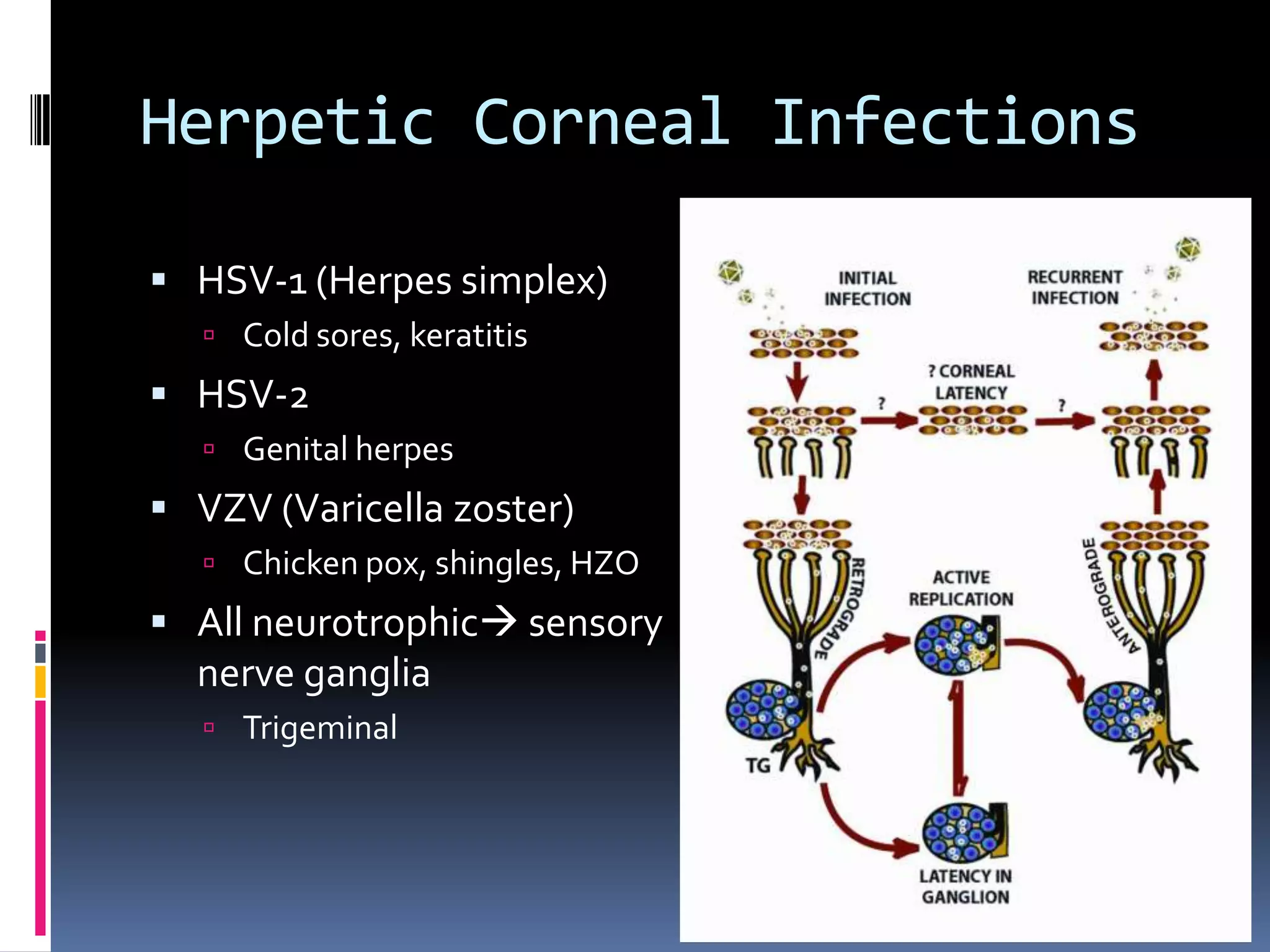
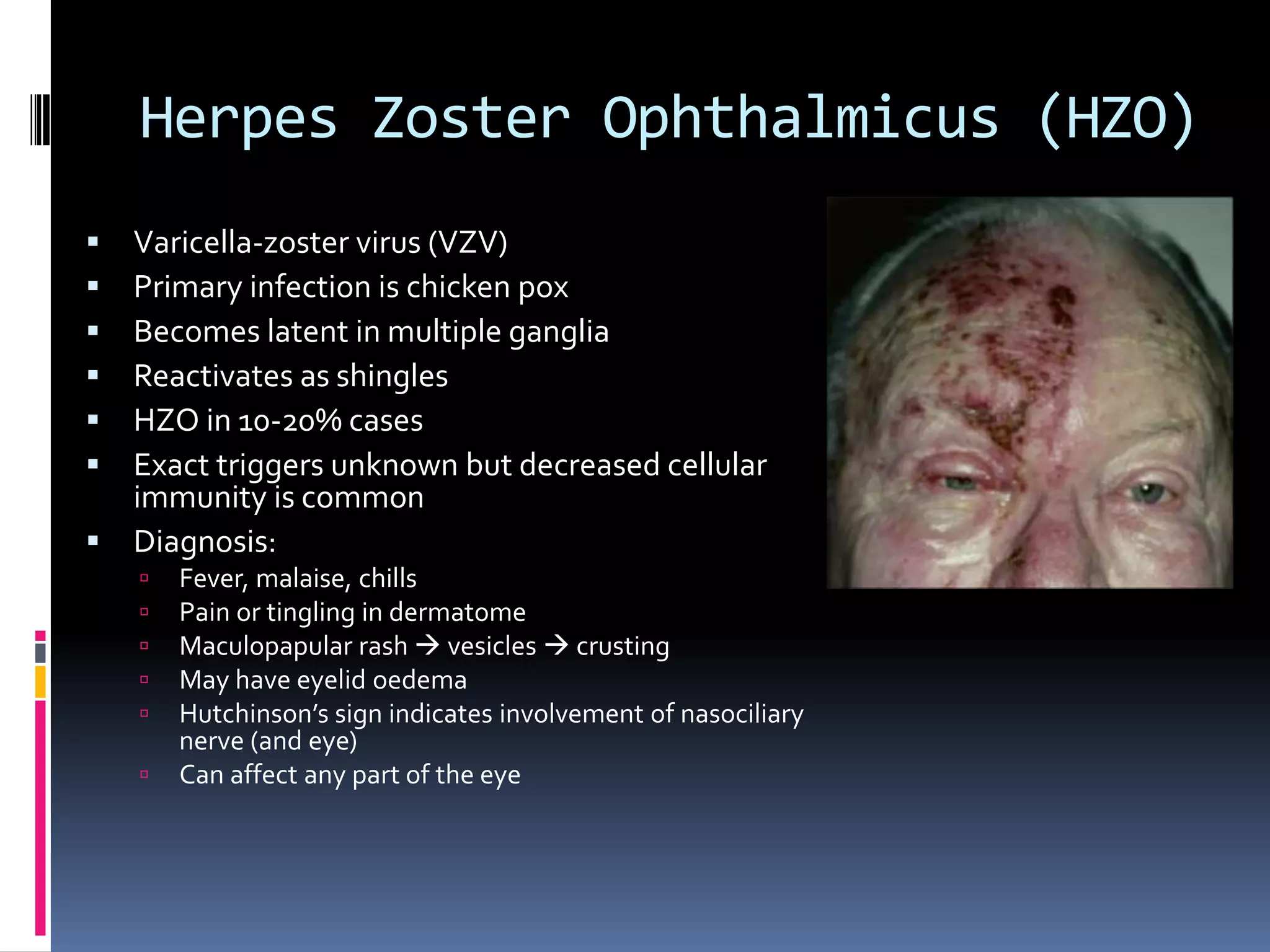
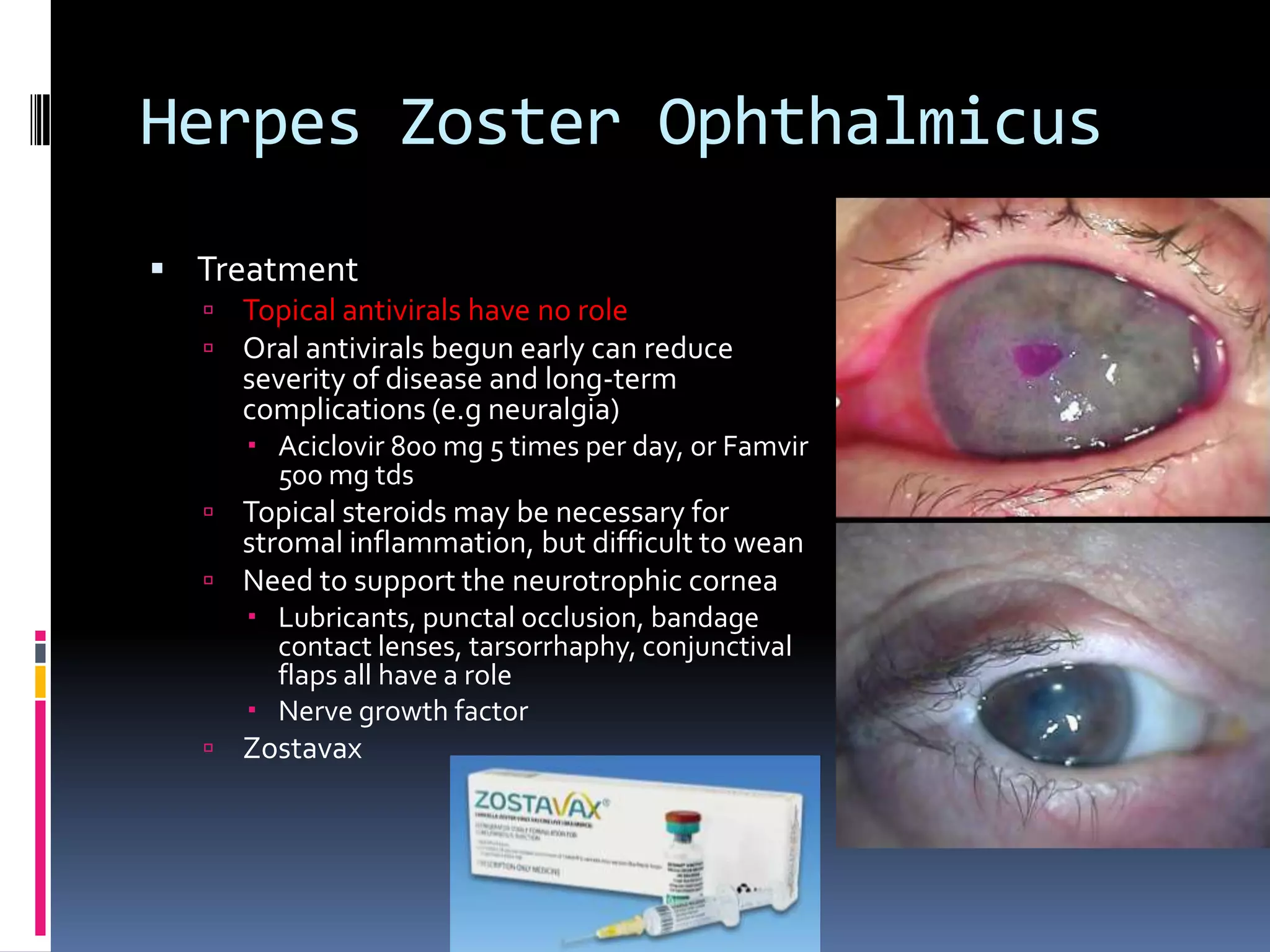
Dr Doug Parker gave a presentation on herpetic corneal disease. He discussed how herpes simplex virus (HSV) and varicella zoster virus (VZV) can infect the cornea and cause disease. HSV typically causes epithelial dendritic ulcers or stromal keratitis, while VZV causes herpes zoster ophthalmicus. Treatment involves antiviral medications, with steroids also used for stromal inflammation. Reduced corneal sensation is a sign of previous herpetic disease and risks neurotrophic ulcers.