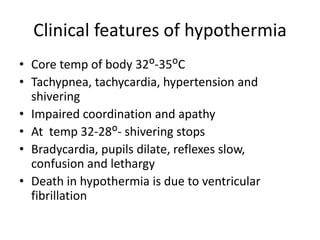
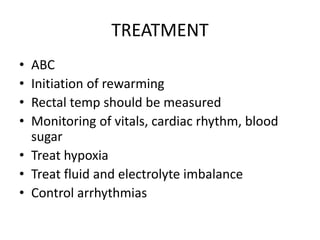
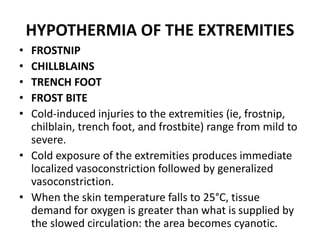
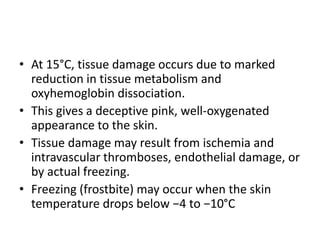
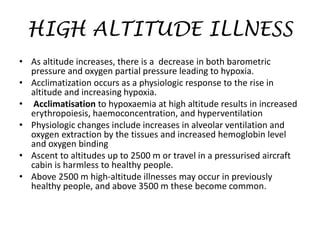
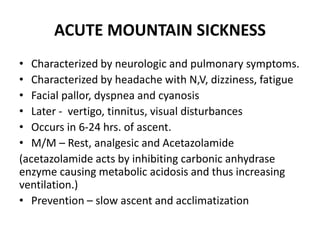
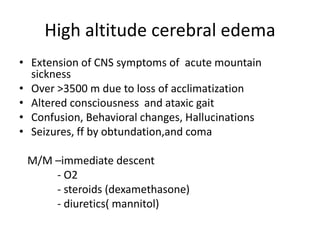
Disorders related to environmental factors can cause hypothermia or hyperthermia. Hypothermia occurs when the body fails to produce enough heat in cold environments, lowering the core temperature below 35°C and impacting various bodily functions. It is common in infants, elderly people, and those with certain medical conditions. Treatment involves slowly rewarming the body and addressing complications. Extremities can also be affected by cold injuries like frostnip, trench foot or frostbite. High altitudes can cause illnesses due to reduced oxygen levels like acute mountain sickness, high altitude cerebral edema, or high altitude pulmonary edema. Radiation exposure depends on various factors and can cause early effects like nausea or long term effects like cancer depending