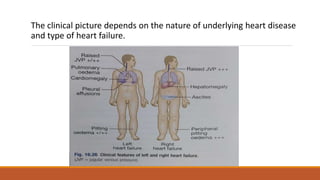
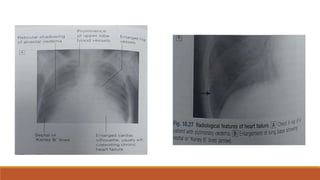
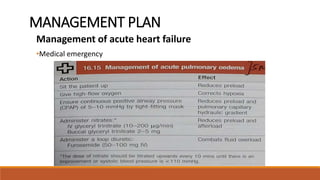
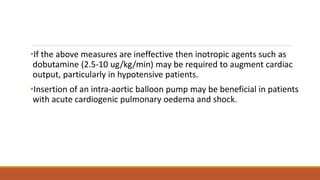
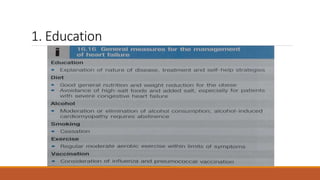
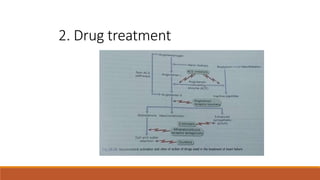
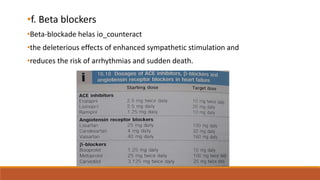
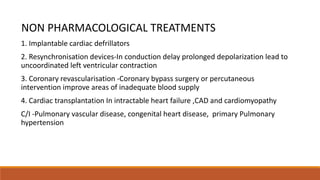
Heart failure is a clinical syndrome arising when the heart fails to maintain adequate output, categorized into left heart, right heart, and biventricular failure, with various causes including reduced contractility and volume overload. Diagnosis involves clinical assessment and investigations such as chest X-ray and echocardiography, while management focuses on medication, lifestyle changes, and in severe cases, non-pharmacological treatments like cardiac devices or transplantation. Complications can include renal failure and arrhythmias, necessitating careful monitoring and adaptation of treatment strategies.