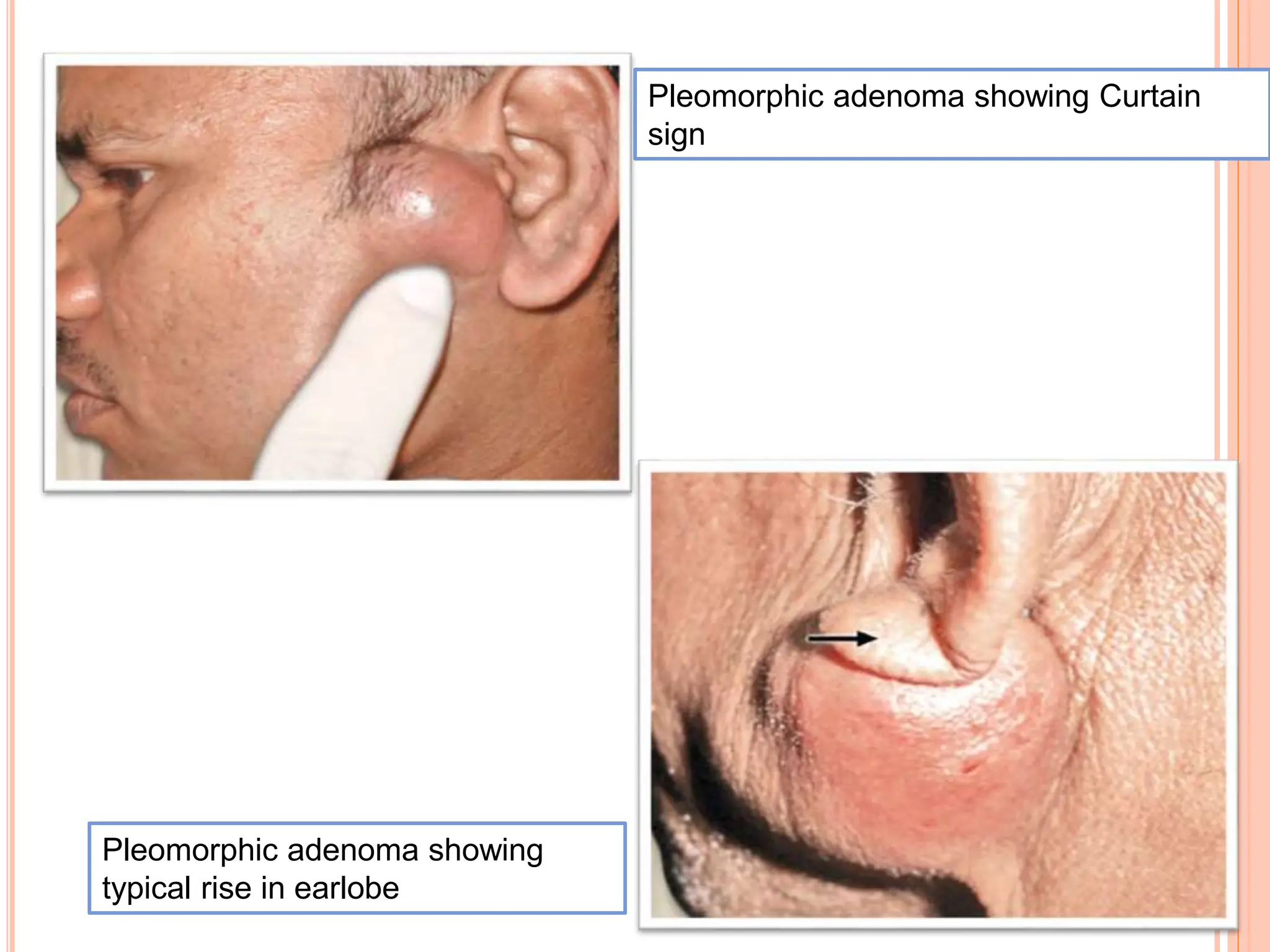
Pleomorphic adenoma is the most common salivary gland tumor in adults, accounting for 80% of such tumors, primarily occurring in the parotid gland. It typically presents as a painless, smooth, and mobile swelling, with potential complications including recurrence and malignancy in some cases. Diagnosis involves fine needle aspiration cytology, while management primarily includes surgical intervention.