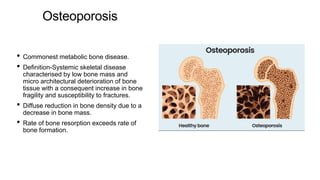
Osteoporosis is the most common metabolic bone disease characterized by low bone mass and increased fragility, leading to a higher susceptibility to fractures, particularly in the dorsal spine. It can be classified into primary and secondary osteoporosis, with various causative factors including aging, hormonal changes, and certain chronic illnesses or medications. Prevention and treatment involve lifestyle modifications, pharmacological interventions like bisphosphonates, and surgical options for advanced cases.