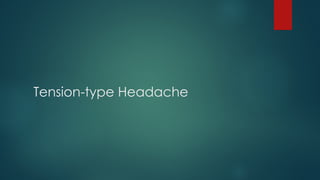
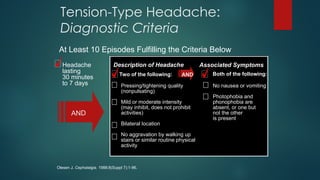
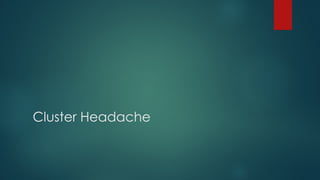
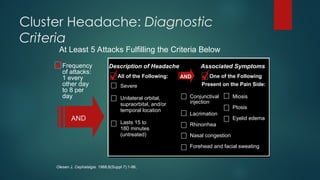
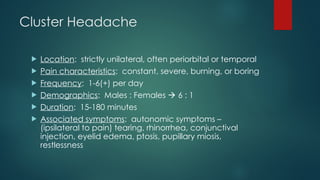
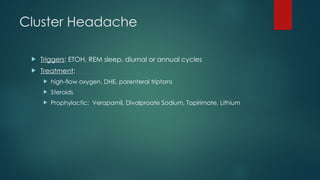
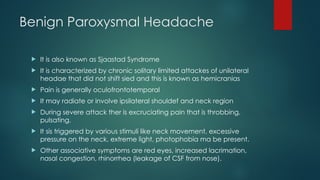
The document provides a comprehensive overview of headaches, detailing their types, prevalence, and defining characteristics, focusing particularly on migraine headaches. It discusses the pathophysiology, classification, and various treatment options including acute and preventative therapies. Additionally, the document outlines medication overuse headaches and other specific headache types such as tension-type, cluster, and benign paroxysmal headaches.

![Introduction
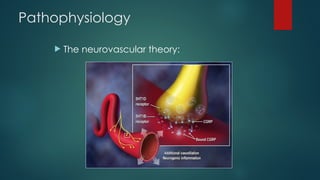
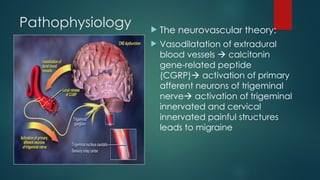
NO pain receptors in the parenchyma [the brain tissue itself]
Pain receptors ARE present in:
Blood vessels
Meninges
Scalp
Skull
Pain sensitive structures are supplied by upper cervical nerves and
trigeminal nerve.](https://image.slidesharecdn.com/headaches-240911024822-bd1cef99/85/Headaches-and-management-physiotherapy-ppt-2-320.jpg)
![Migraine
Migraine without aura [common migraine]
Migraine with aura [classic migraine]](https://image.slidesharecdn.com/headaches-240911024822-bd1cef99/85/Headaches-and-management-physiotherapy-ppt-10-320.jpg)