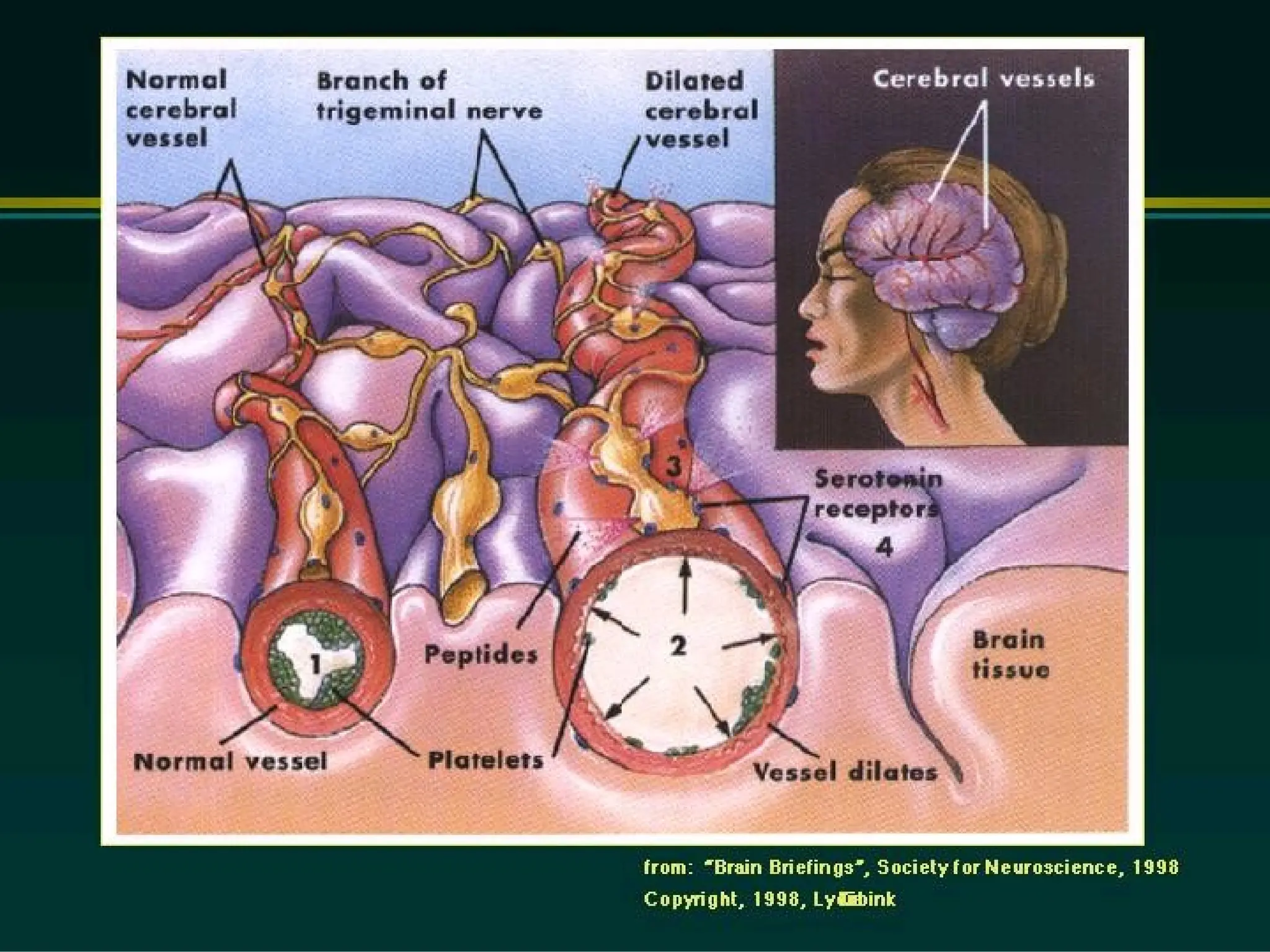
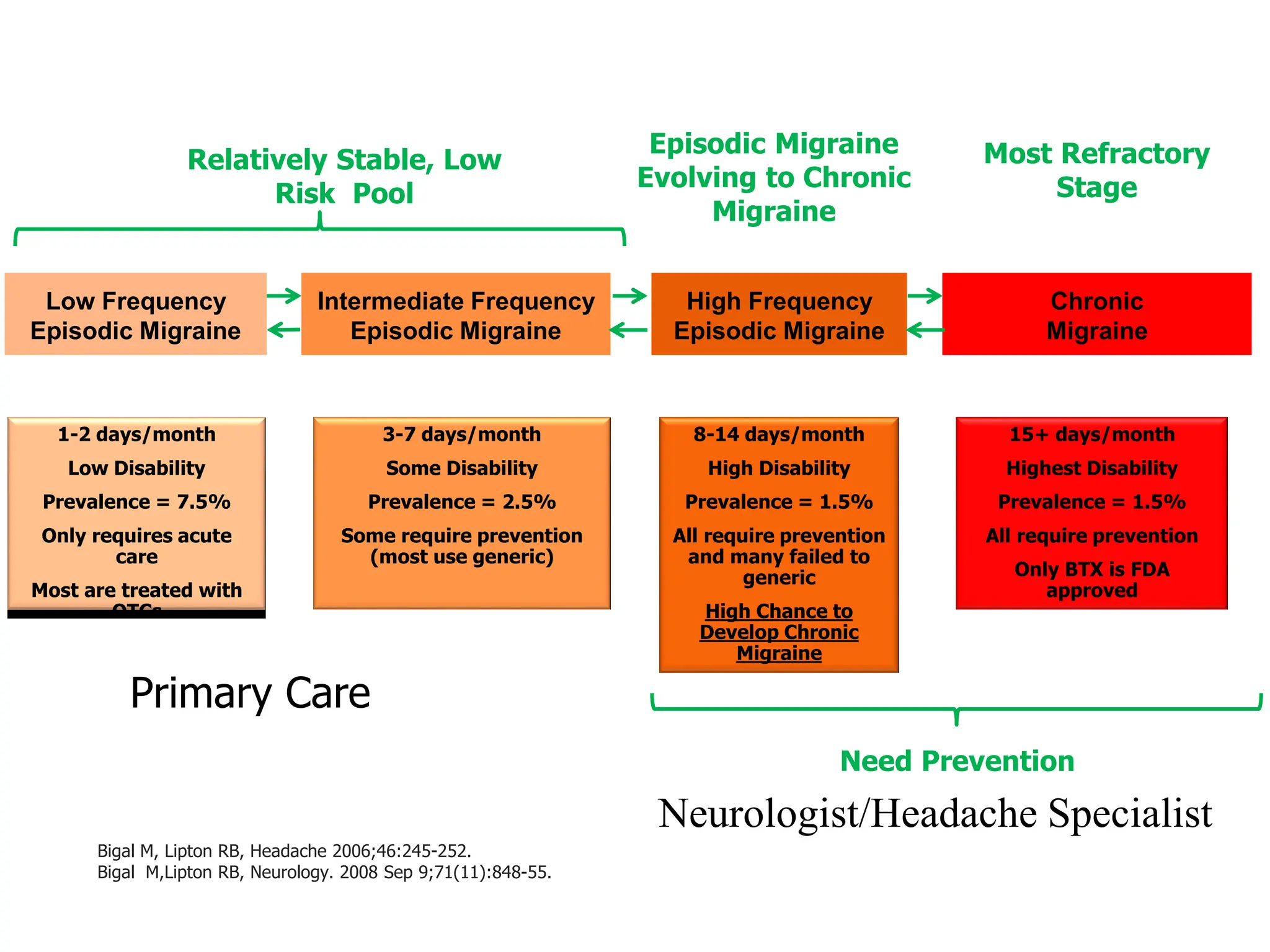
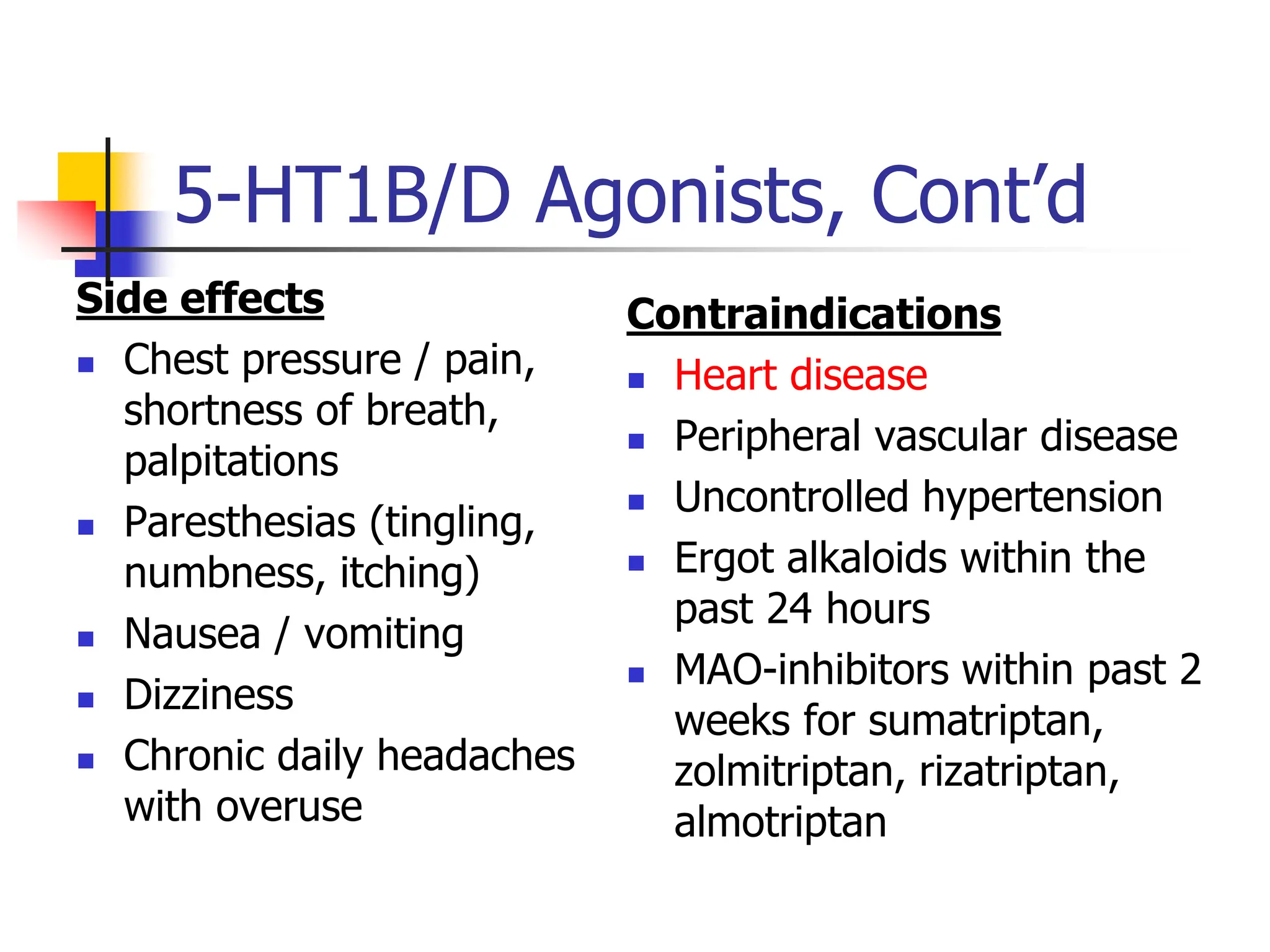
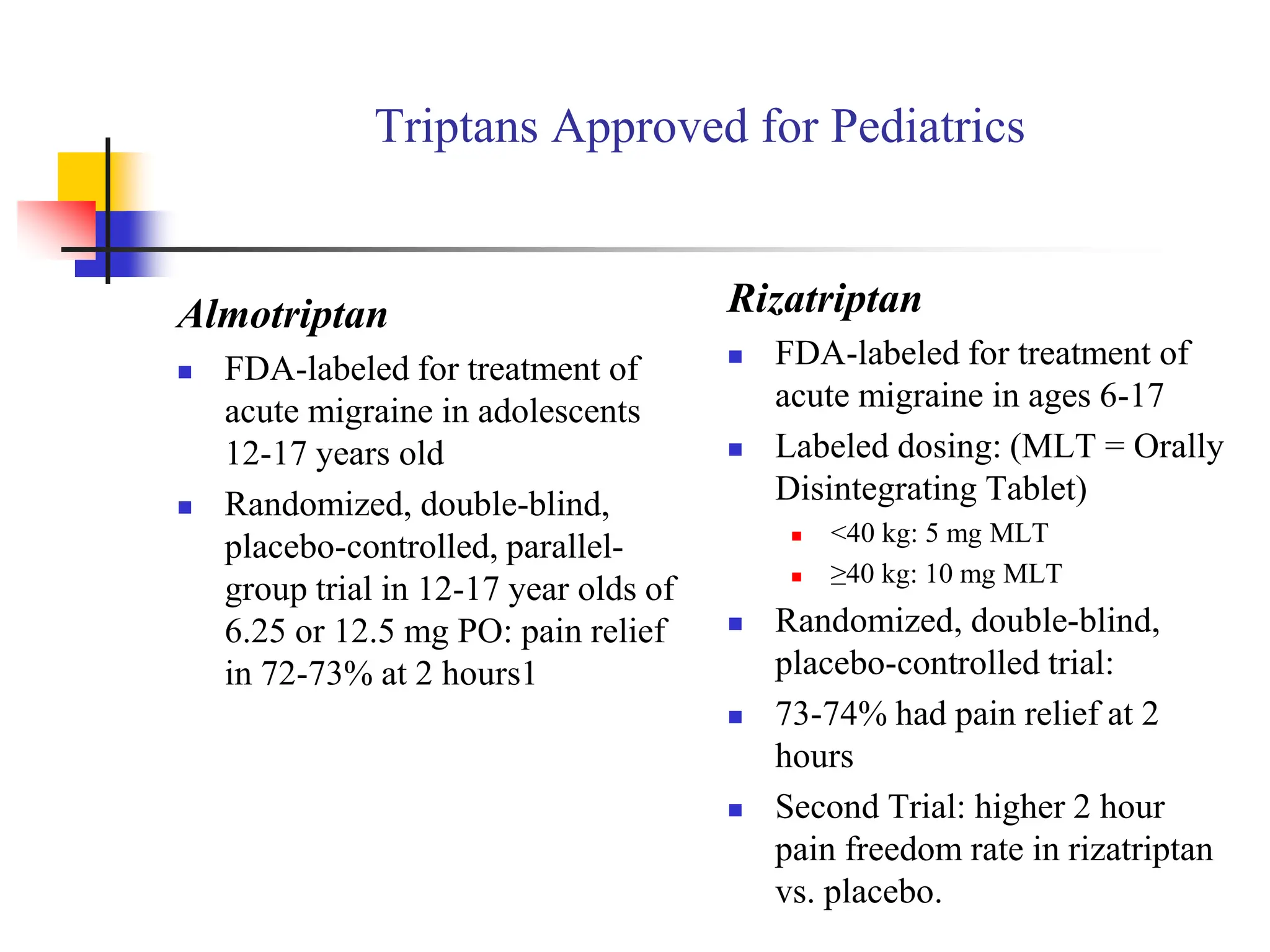
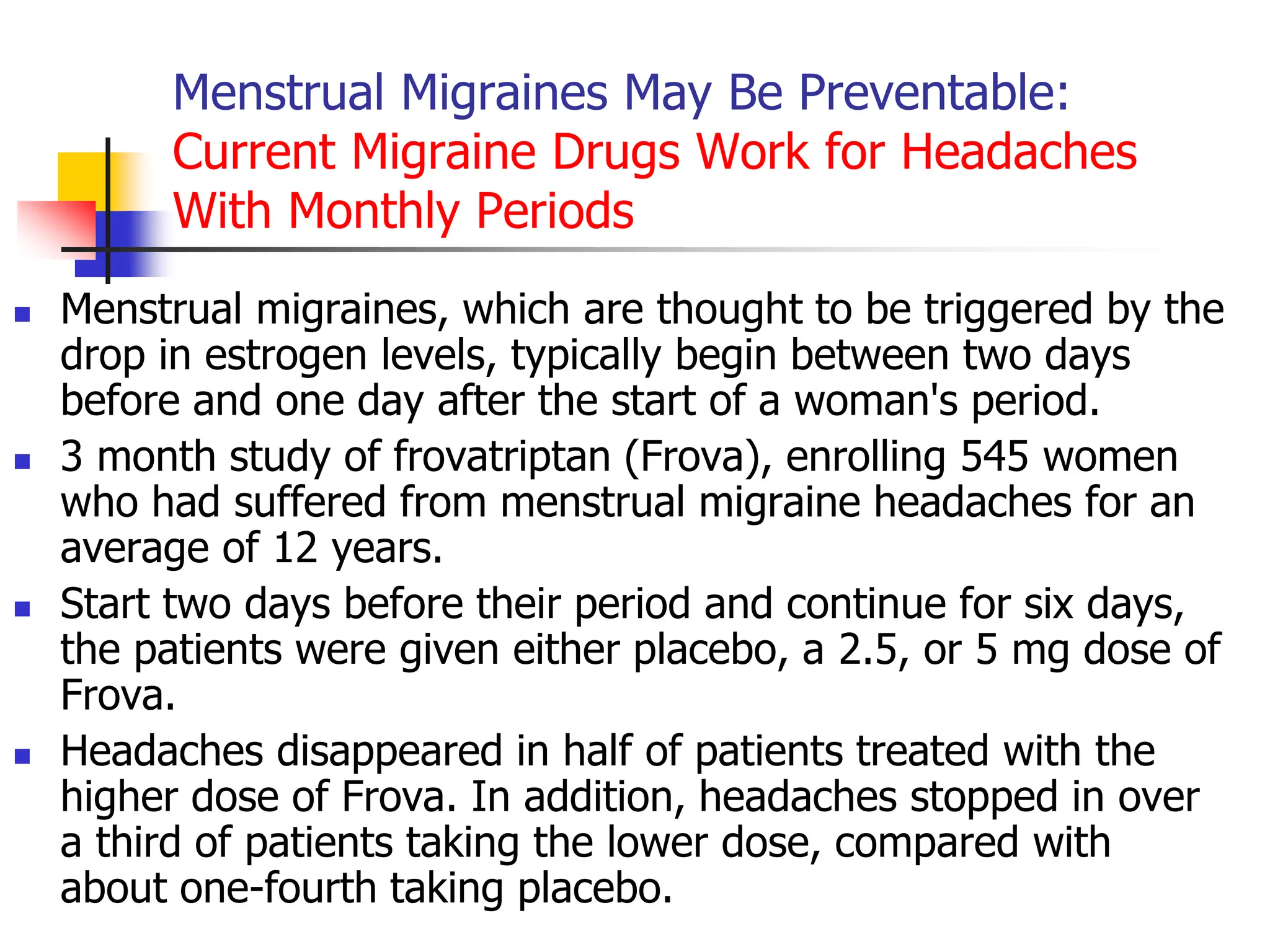
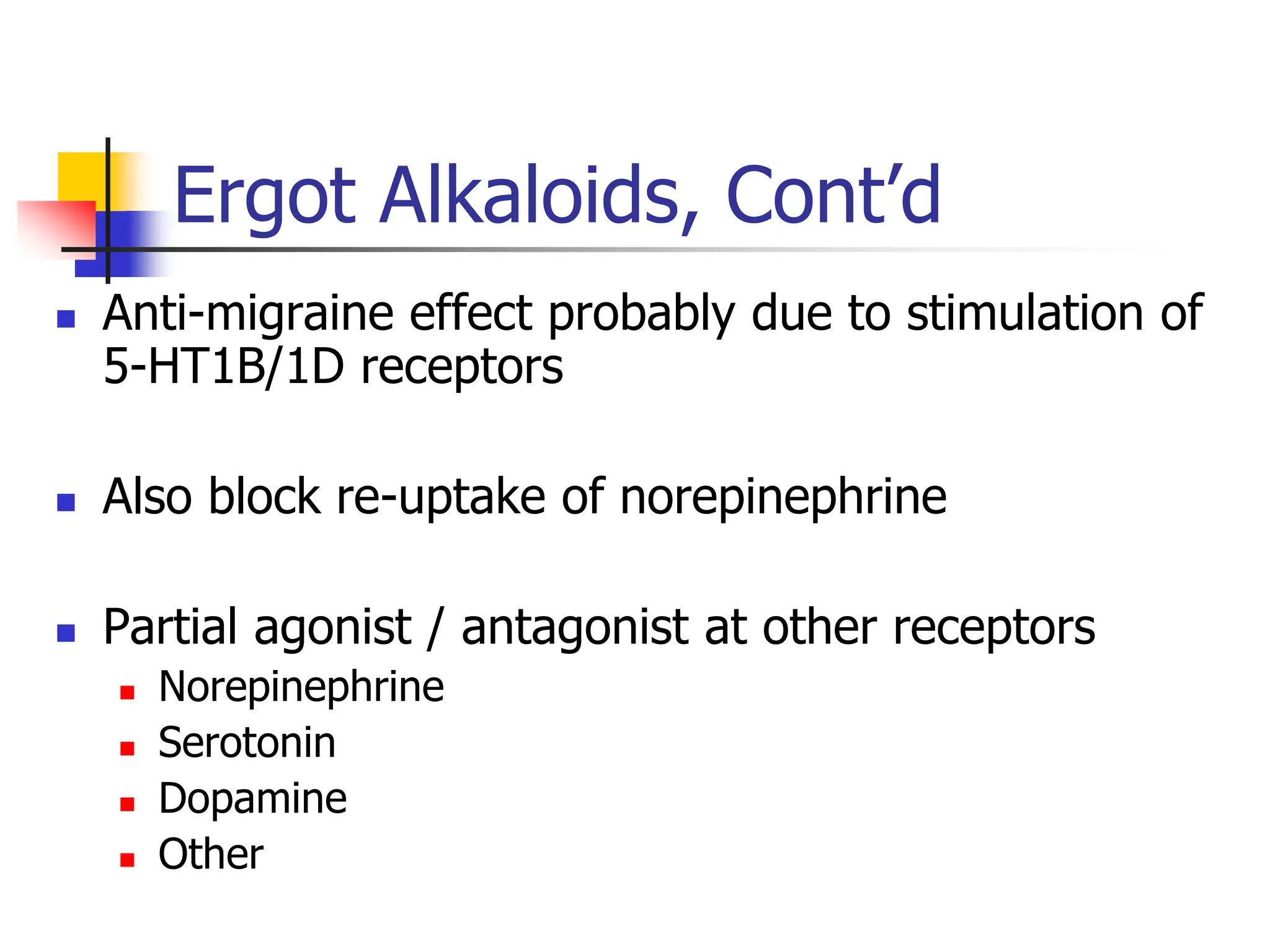
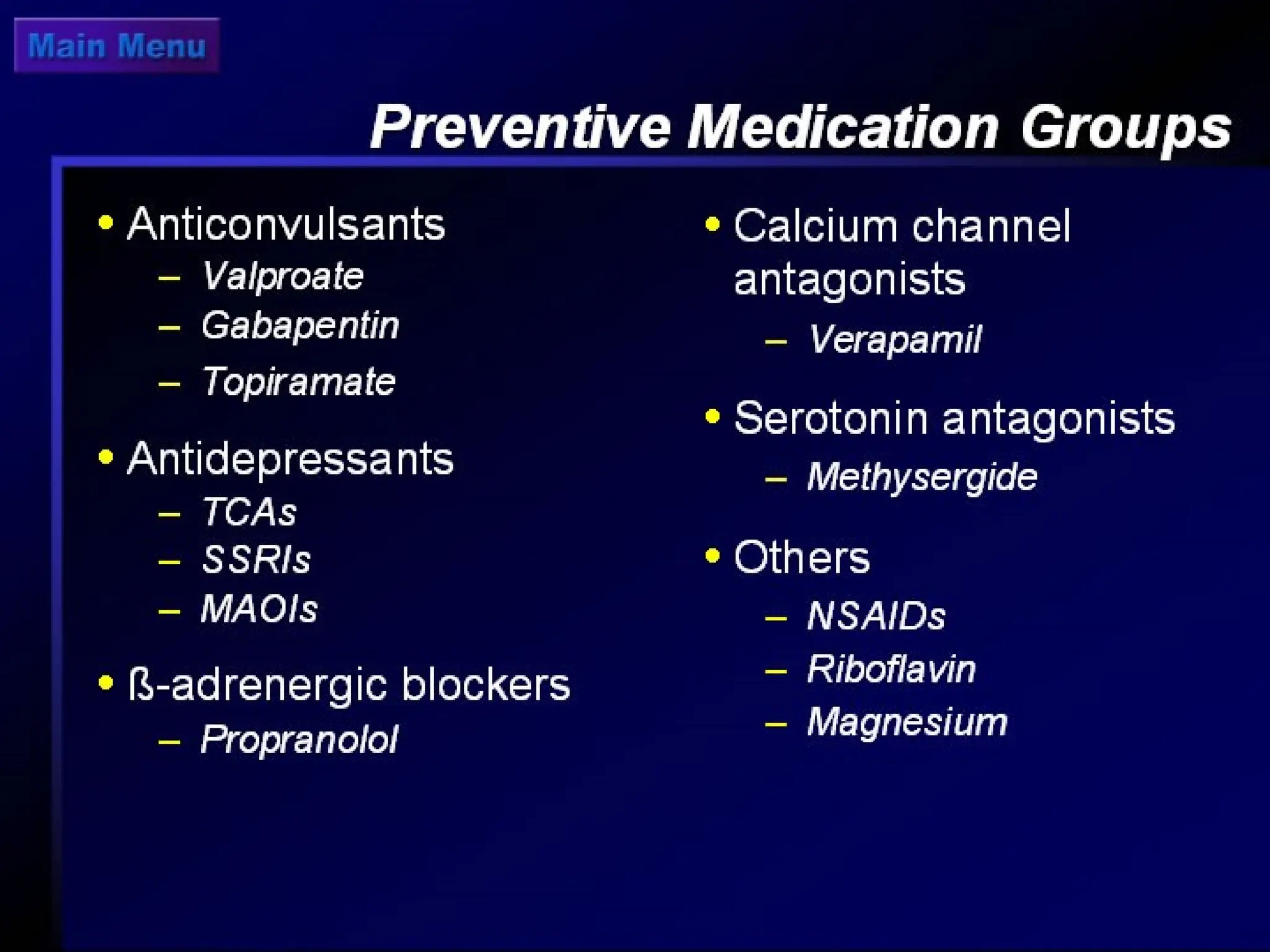
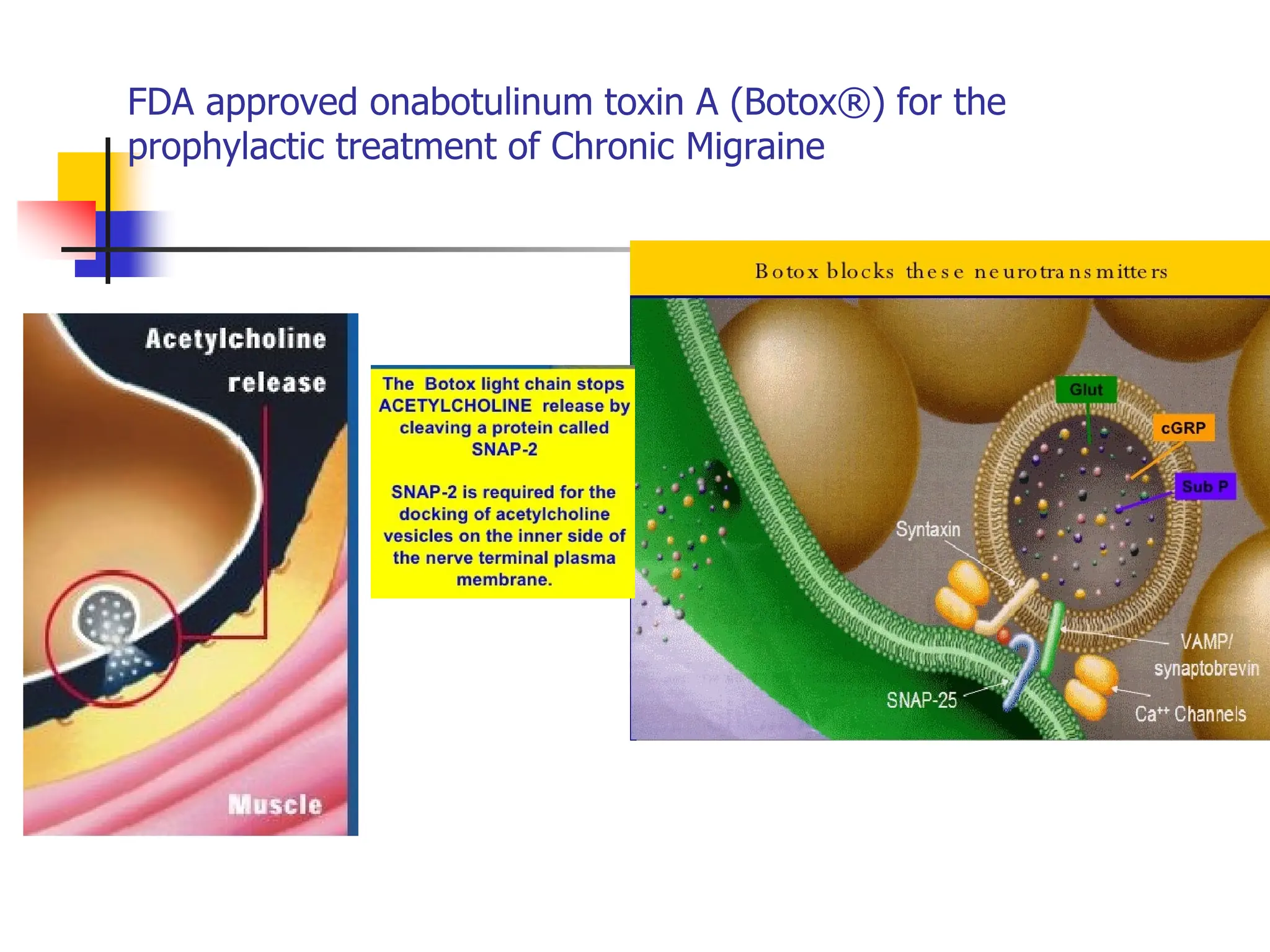
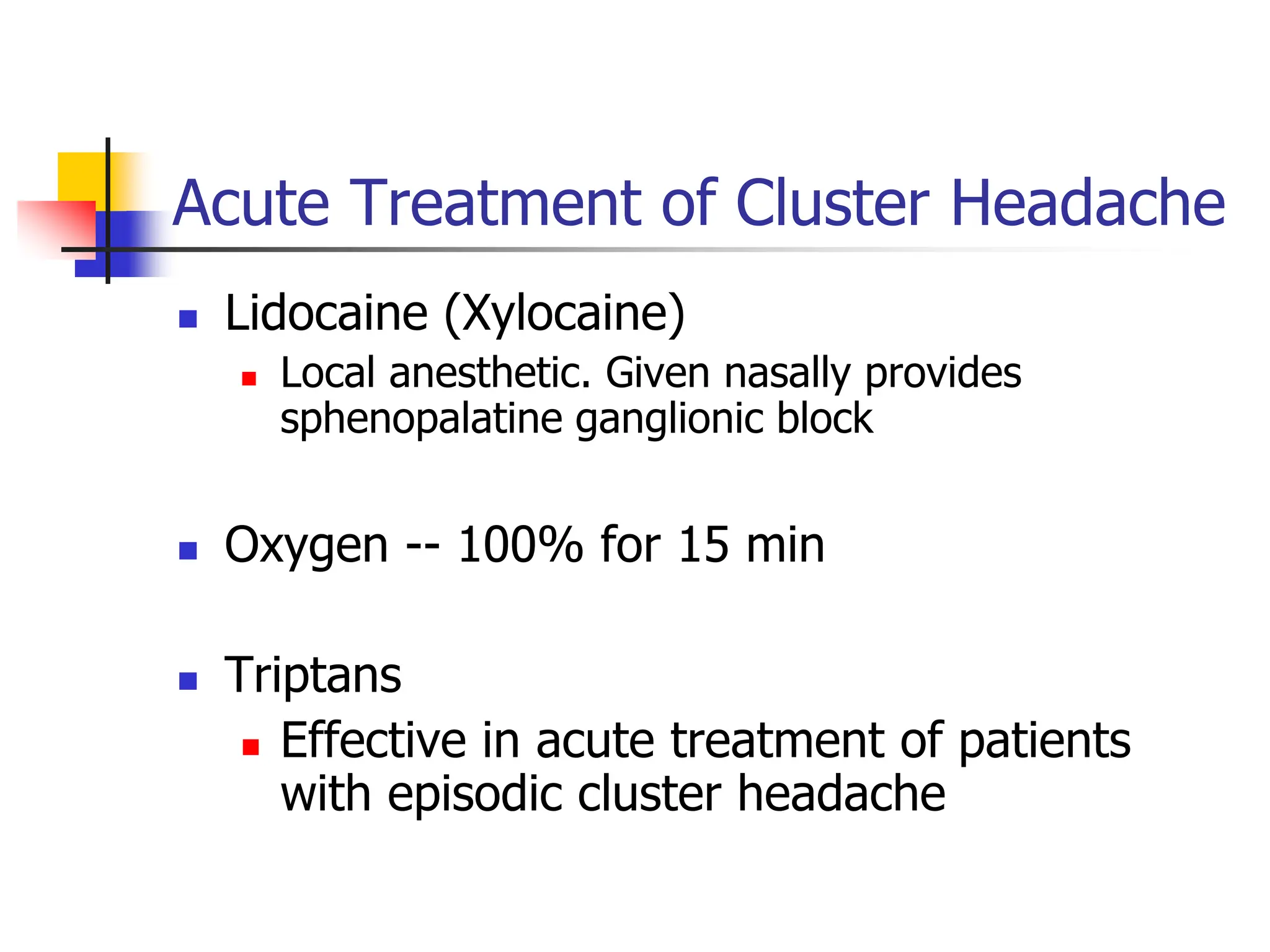
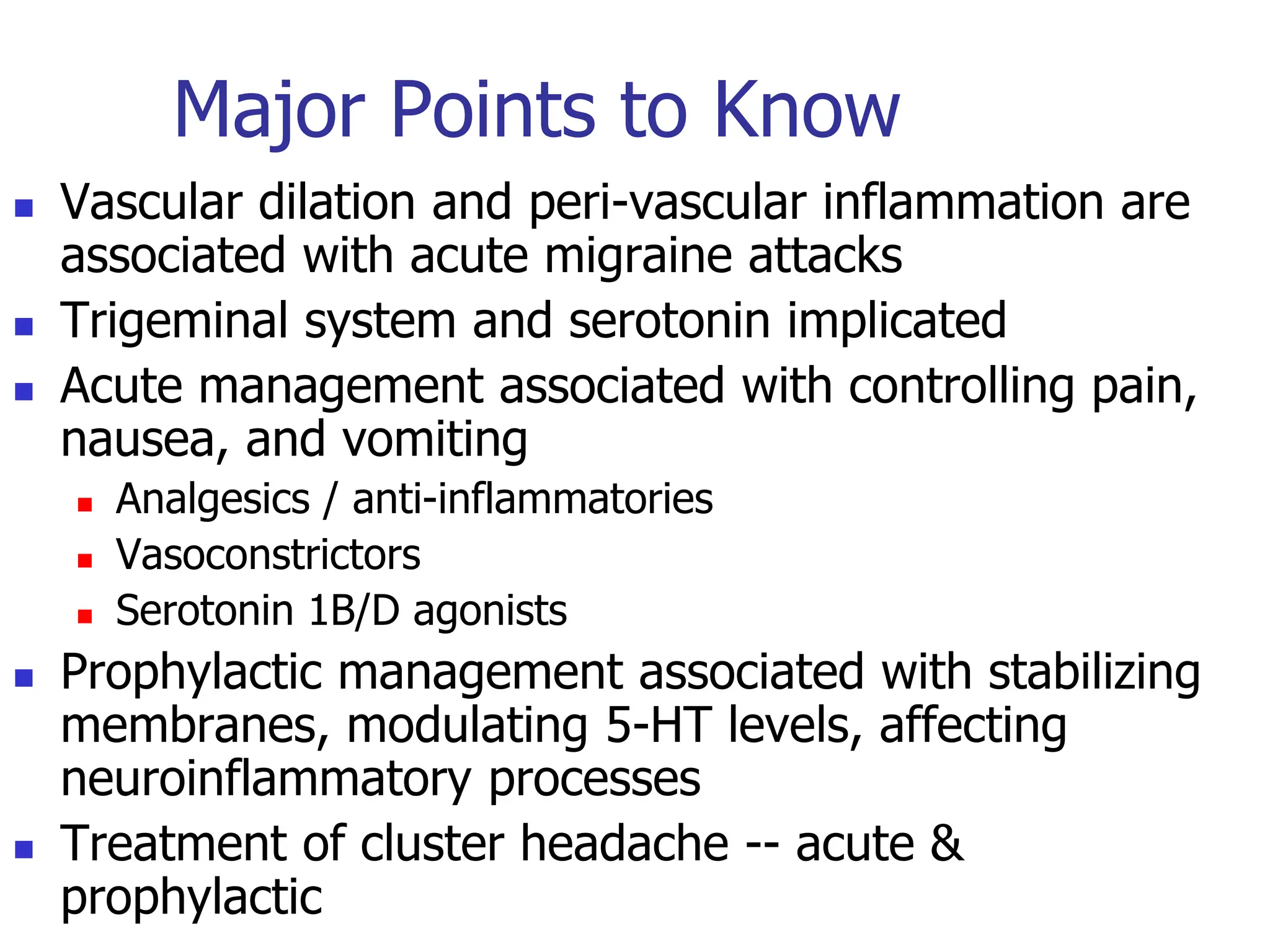
Migraine, tension, and cluster headaches have distinct characteristics but share some common treatment approaches. Acute migraine is treated with analgesics, anti-inflammatories, vasoconstrictors, and serotonin agonists to control pain, nausea, and vascular changes. Prophylactically, medications aim to stabilize neuronal membranes, modulate serotonin levels, and affect neuroinflammation. Cluster headaches are treated acutely with oxygen and lidocaine and preventatively with verapamil, lithium, and prednisone.