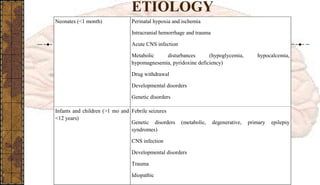
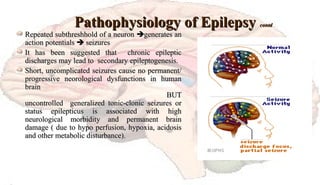
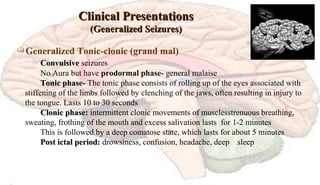
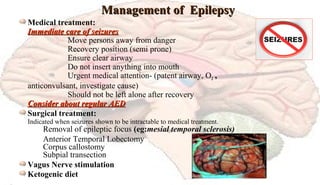
This document provides information on the management of patients with epilepsy. It defines epilepsy and seizures, discusses the difference between seizures and epilepsy, and covers the historical background and classifications of seizures. It also discusses the causes, pathophysiology, clinical manifestations, diagnosis and management of epilepsy. Management involves treatment of acute seizures, removal of precipitating factors, long-term antiepileptic drug therapy, and other options like surgery or diet. The goal of management is to control seizures and prevent complications through appropriate treatment.